INTRODUCTION
The phenomenon of the establishment of a zone of biologic width (BW) is an important clinical concept in restorative dentistry and periodontics for many years.1, 2 The supracrestal soft tissue attachment of the periodontal tissues to the tooth/root surface has been termed as the BW.3 In other words, BW refers to the height of the dento-gingival attachment apparatus necessary for a healthy existence of bone and soft tissue from the most apical extent of a dental restoration. The dimensions of the BW having an average value of 2. 04 mm is considered to be norm for most patients and most teeth, although significant variations especially in the length of the epithelial attachment can occur.1, 4
Although supracrestal connective tissue attachment is variable in nature, this component of the periodontal support that may provide periodontal stability to teeth that lack alveolar bone support as well as providing an unusually large BW.5 But these values of BW measurements should not be extrapolated for use in pathologic situations as they were taken from healthy periodontium.6 It has been believed for many years that the distance from the base of the sulcus to the crest of the alveolar bone remains generally constant, with mean values of 1.94 to 1.97 mm.7,8
Periodontal disease is generally chronic in nature and shows slow progression. Various factors such as host- bacterial interaction, various environmental factors, acquired risk factors such as systemic diseases and conditions, smoking and in some cases altered expression of inflammatory genotype are the causes for progression of the disease resulting in severe bone and attachment loss at an early age.6
A variation in BW in cases of periodontitis provides significant implications for the selection of surgical or non-surgical approaches. Various studies have reported that surgical intervention in sites with shallow probing depths resulted in post-surgical loss of attachment at that site.9-14 Very few studies have evaluated the dimension of BW in humans with clinically diagnosed periodontitis.15 So, the purpose of the present study is to determine whether the previously evaluated histologic dimensions of the BW apply in untreated cases of chronic generalized periodontitis and to understand the influence of these BW variations on approach to therapy.
METHODS AND MATERIALS
A total of 54 subjects (37 males and 17 females) between the age ranging from 30 to 60 years were enrolled in this cross-sectional study conducted over a period of one year at outpatient Department of Periodontology, Yenepoya Dental College, Mangalore. The study protocol was approved by Ethics Committee of the university and informed consent was obtained from all the patients. All patients were provided with verbal explanation of the nature of the study. The following inclusion criteria were considered: Subjects with clinically healthy periodontium constituted group A, subjects with chronic generalised periodontitis constituted group B and each subject having at least 20 erupted natural teeth. Exclusion criteria included subjects: 1) with systemic diseases; 2) taking antibiotic therapy within the past 3 months; 3) who received non-surgical periodontal therapy 3 months prior to study; 4) who received surgical periodontal therapy in the past 12 months; and 5) pregnant females.
Data was collected by performing clinical and radiographic examination to determine clinical BW. For each patient, the periodontal examination was performed by a single examiner, and following parameters such as Gingival index (Loe and Silness 1963), Community periodontal index (CPI), full- mouth recording of probing depths (PDs) and clinical attachment levels (CALs) at six sites per tooth, except third molars were recorded using a millimetre calibrated University of North Carolina (UNC) 15 probe (Figure 1).16, 17

|
Figure 1: Armamentarium
Click here to view |
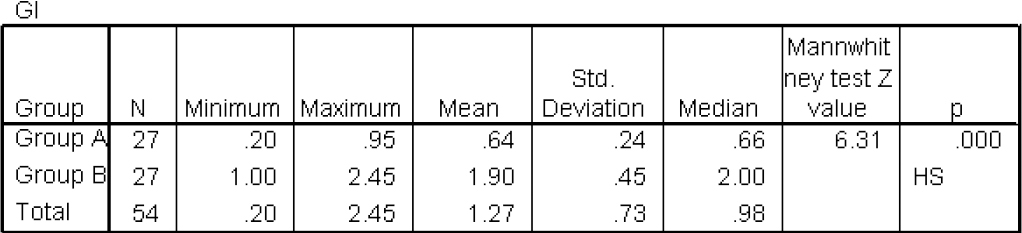
The clinical biologic width was determined from the most coronal level of clinical attachment to the crest of the alveolar bone on proximal surfaces. Full mouth series of periapical radiographs were taken for each subject using the long cone paralleling technique by Satelec Acteon X-mind AC x-ray unit. All radiographs were exposed with settings at 70 kilovolt and 8 mA. IOPA were captured with No. two size, Ektaspeed films (Eastman, Kodak, Rochester, NY, USA) using paralleling technique with the help of Rinn XCP holder (Rinn Corporation, Elgin, Ill, USA) as per the criteria given by Jorgenson T et al.16 The focal spot was concentrated at 0.7mm and the exposure time was set to 0.4 sec. Films were processed under standardized conditions using an Velopex automatic processor. Radiographs were digitized by projecting each x-ray film onto a LED x-ray film viewer. All radiographs were placed in slide holders on a light viewing box and photographed using a Canon IXUS 230 HS digital camera (Canon Inc., NY, USA) with 8x zoom, 28mm wide lens, 12.1 Megapixel High Sensitivity CMOS Sensor and Optical Image Stabiliser with Intelligent IS with a recording image of 1024 x 768 pixels.
The Canon camera images were taken at the same camera-radiograph distance with a mini tripod. Identical illumination was used throughout with the radiographs placed at the same location on the light box (Figure 2). Digital camera images were saved as Joint Photographic Experts Group (JPEG) files. Digital images were loaded directly onto a Lenovo L430 ThinkPad laptop with a 14 inch screen.
|
Figure 2: Digitizing the radiograph
Click here to view |
Images were opened using Micro Dicom viewer software (Version 0.7.7 Sofia, Bulgaria). The full screen was used with a black background for each image.
The radiographs were scanned to obtain digitalized images to measure the crestal bone level (CBL that is the distance from cementoenamel junction (CEJ) to the alveolar crest) on proximal surfaces using computerized software (Figure 3). Only proximal surfaces were used in the analysis, and mean values of the buccal and lingual proximal clinical measures for CAL were used for comparison with BL at each evaluated radiographic surface. Clinical BW is defined as the distance from the most coronal level of the CAL to the CBL. As CEJ is used to calculate CAL and CBL, clinical BW was calculated by subtracting the CAL from CBL.

|
Click here to view |
STATISTICAL SIGNIFICANCE
The data obtained were subjected to descriptive and comparative statistical analysis. Data was summarized as mean and standard deviation for continuous variables. The Student t-test was used for comparing the means of quantitative variables. Chi-square test, Fisher’s exact test and Mann- Whitney U test were used to determine whether the differences in proportions and means were statistically significant. Pearson’s correlation coefficient was computed to measure degree of correlation between PD, CAL, BL and BW. All analyses were performed using Statistical Program for Social sciences Version 20.0 (SPSS) software. The differences were considered to be statistically significant only for p<0.05 and highly significant for p<0.001.
RESULTS
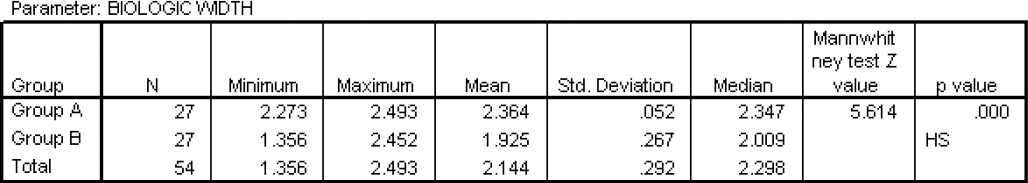
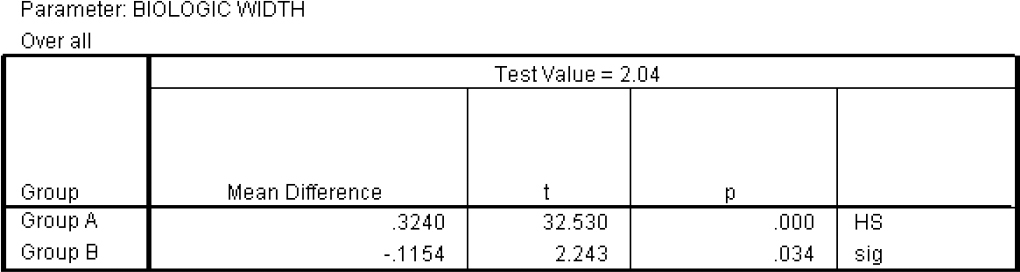
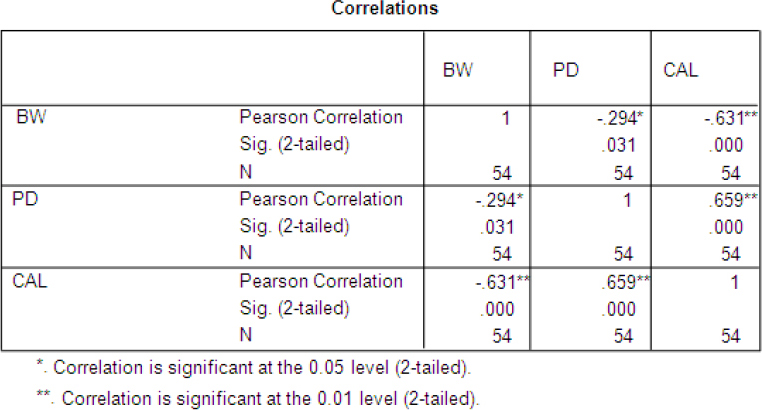
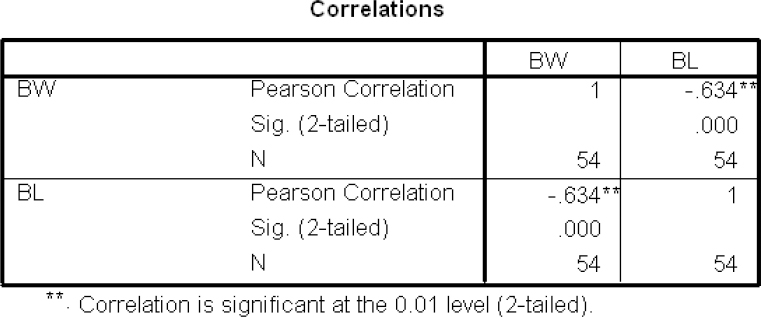
A total of 54 subjects in the age group of 30-60 years were included in the study and the subjects were divided into control group (33.89±4.06) and test group (46.44 ± 7.64). Assuming a · error of 0.05 and 95% confidence interval, the power of the study was found to be 80%. Table 1 reveals that the mean gingival index scores were significantly higher in group B compared with group A (p < 0.001). The results of Community Periodontal Index (CPI) showed that code 1, 2, 3, 4 was found to be statistically significant because p value was 0.0001 for all the codes respectively (Table 2). The results of clinical attachment loss (CAL) showed that code 0, 1, 2, 3, 4 were statistically significant because p value was 0.0001 respectively. CPI Code 1 was more in group A whereas code 2, 3, 4 was more in group B suggestive of periodontally healthy subjects in group A and subjects with chronic periodontitis in group B (Table 3). The results showed that for all evaluable proximal sites, mean clinical biologic width in healthy subjects was significantly higher than mean clinical biologic width in subjects with chronic generalized periodontitis (p < 0.001) as represented in table 4. The results showed that mean clinical biologic width in group A was significantly higher than previously reported biologic width (p < 0.001) whereas mean clinical biologic width in group B was found to be significantly lower than previously reported biologic width (p = 0.034) as represented in table 5. For all sites combined, Pearson’s correlation (r) in table 6 shows a significant positive correlation (p < 0.001) between PD and CAL. Further, a negative correlation was found between BW, PD and CAL (p < 0.05). A negative correlation was found between BW and BL, which was statistically significant (p < 0.001) (table 7).
|
Table 1: Mean Gingival Index of Test group and Control group
Click here to view |
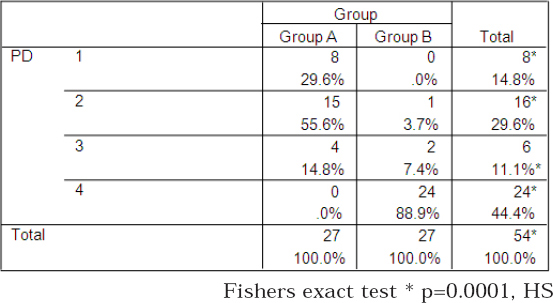
|
Table 2: Distribution of subjects according to the Community periodontal index CPI codes in relation to probing depth
Click here to view |
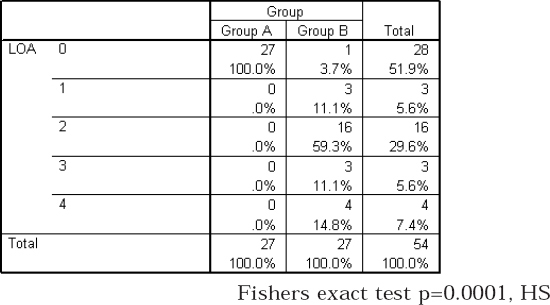
|
Table 3: Distribution of subjects according to the Community periodontal index CPI codes in relation to loss of attachment
Click here to view |
|
Table 4: Comparison of mean and standard deviation of clinical biologic width in group A and group B
Click here to view |
|
Table 5: Comparison of clinical biologic width of group A and group B with previously reported biologic width
Click here to view |
|
Table 6: Correlation between BW,PD & CAL
Click here to view |
|
Table 7: Correlations between BW & BL
Click here to view |
DISCUSSION
The present study was aimed to compare clinical BW in chronic periodontitis and periodontally healthy subjects with previously reported histologic BW. The study design involved patients with chronic generalized periodontitis (n = 27) and healthy subjects (n = 27). The study included measurement of clinical parameters and radiographic parameters.
The biologic width is defined as the dimension of the soft tissue, which is attached to the portion of the tooth coronal to the crest of the alveolar bone. This term was based on the work of Garguilo et al (1961) who measured dentogingival components in 287 individual teeth from 30 autopsy specimens and established that there is definite proportional relationship between alveolar crest, the connective tissue attachment, the epithelial attachment and the sulcus depth. They determined that the epithelial attachment length was 0.97 mm, and the connective tissue attachment length was 1.07 mm, so the combined dimension of the connective tissue attachment and the junctional epithelium (the normal biologic width) averages 2.04 mm in a healthy periodontium. The most constant part of dentogingival junction dimension was the connective tissue attachment and the most variable part was the epithelial attachment.[4] The histologically determined the biologic width in adult human cadaver jaws obtained measurements of 1.14 ± 0.49 mm for epithelial attachment, 0.77 ± 0.32 mm for connective tissue attachment, 2.17 mm for biologic width, 1.07 mm for junctional epithelium, and 1.10 mm for the connective tissue were reported by Vacek et al (1994) and Xie et al (2007).18,19
There are no comprehensive evaluations of BW in advanced cases of periodontitis where significant changes in connective tissue and bone have occurred. Therefore, the present study took advantage of baseline data obtained as part of an intervention in subjects with chronic generalized periodontitis to examine the changes in BW that might occur in periodontitis. In the present study, the first observation was that the average clinical biologic width in cases of chronic generalized periodontitis was 1.92 mm, which was lower than the histologic biologic width previously reported for subjects not demonstrating significant periodontal pathology. Mean clinical biologic width in group B was found to be significantly lower than previously reported biologic width (p=0.034). Papananou et al (1989) reported strong correlation (r=0.80) between radiographic assessment of alveolar bone loss and changes in CAL.20 Also, Clerehugh & Lennon (1986)[21] reported a similar correlation (contingency coefficient of 0.51).21 Conversely, Goodson et al (1993), Mann et al (1985) and Machtei et al (1997), in a similar study of the relationship between clinical and radiographic detection of periodontal disease progression, reported poor agreement between the two variables.22-24
It was seen that the mean clinical biologic width in subjects with healthy periodontium (2.36 mm) was significantly greater than the mean histologic biologic width reported previously (2.04 mm). Similar observations were made by Novak et al (2008) and Gaddale et al (2015) Alpiste-Illueca et al (2004), Al-Rasheed et al (2005), Galagali and Gontiya et al (2012) obtained mean biologic of 2.00 +/-0.72, 1.24 mm and 1.72 mm.15, 25-28 For all evaluable proximal sites, the mean clinical biologic width was 2.14 mm versus the mean histologic biologic width of 2.04 mm which is consistent with the findings of previous studies done by Novak et al (2008) and Gaddale et al (2015).5, 25 These results corroborate the notion that the dimensions of the dentogingival unit are highly variable in humans. The dimensions of biologic width seem to differ with respect to periodontal health and in untreated chronic periodontitis patients.
An examination of correlation coefficients confirmed our initial observations that for sites with chronic periodontitis, CAL was significantly correlated with BL and showed an inverse relationship with BW which means as CAL and BL increases, BW decreases. This was observed as bone levels are used in the determination of the BW. Also, the results showed that sites with shallow PDs and least CAL had the greatest BW in case of healthy subjects. This observation provides significant implications for the selection of surgical or non- surgical approaches in the treatment of patients with chronic periodontitis.
In our study, mean gingival index for the chronic periodontitis group was higher compared to the control group, which was statistically highly significant (p<0.001). This finding is in accordance with previous studies done by Lang et al (1990), Albandar et al (1998), Schatzle et al (2003).29-31 Claffey et al (1995) reported that for higher risk patients, bleeding on probing at maintenance examinations may be a useful indicator of subsequent deterioration at a site level.32
In the present study, distribution of subjects according CPI index codes 1 and 2 in relation to PD and CAL was higher in healthy subjects than chronic periodontitis group, which was statistically highly significant (p < 0.001) and distribution of subjects according CPI index codes 3 & 4 in relation to PD and CAL was higher in chronic periodontitis group as compared to healthy subjects, which was statistically highly significant (p < 0.001). These findings are similar to the studies conducted by Brown at al (1993), Kaimenyi et al (1982), Pilot et al (1986), Benigeri et al (2000).33-36
Results also showed that there was no statistical difference between studied groups in relation to smokers (p=0.054). There were 57.4% non-smokers and 42.6% smokers among group A and group B respectively.
CONCLUSION
Within the limitations of the study, it may be concluded that clinical BW in chronic periodontitis patients was significantly lower than the previously reported histologic BW. Mean clinical BW was significantly higher than previously reported histologic BW. Thus, there is significant intra- and inter individual variability in the dimensions of the biologic width. The dimensions of the biologic width seem to be affected by periodontal diseases.
