INTRODUCTION
Periodontal diseases, a series of infections of the periodontal tissues which eventually can lead to loss of teeth, are form of aberrant inflammation.1 The release of inflammatory mediators and cytokines as local host response to the periodontopathic bacteria appears to play crucial roles in the pathogenesis of periodontal diseases.1 Many biological events are strictly regulated by cell-cell interactions, which may be either cognate (adhesive) interactions, achieved by membrane-bound cell-surface molecules; or cytokine-mediated interactions. Cytokines are small soluble proteins produced by a cell that alter the behavior or properties of another cell locally or systemically in an autocrine or paracrine manner. They are pleiotropic molecules and most of them are multifunctional. Cytokines are involved in extensive networks that involve synergistic as well as antagonistic interactions and exhibit both negative and positive regulatory effects on various target cells.1These play an important role in numerous biological activities including proliferation, development, differentiation, homoeostasis, regeneration, repair and inflammation.2
Thus, the investigation of interleukins responses to periodontal diseases is at the forefront of the translational research agenda in oral science. This review summarizes interleukin expression in periodontal tissues and its importance in tissue homeostasis and, in particular, in the pathogenesis of periodontal diseases.
Interleukins are a large group of immunomodulatory proteins that elicit a wide variety of responses in cells and tissues. Interleukins initiate a response by binding to high-affinity receptors located on the surface of cells; Interleukins function in a paracrine or autocrine fashion, rather than as an endocrine signal, which is more common with steroidal and amino acid-derived hormones. The response of a particular cell to these cytokines depends on the ligands involved, specific receptors expressed on the cell surface and the particular signalling cascades that are activated. ILs modulate growth, differentiation and activation during an immune response. This distinguishes them from chemokines - the main function of which is to direct immune cells to the site of inflammation via chemotaxis - and interferons (IFNs) , which predominantly mediate cellular response to viral infection.
The Nomenclature of Interleukins
The term interleukin derives from (inter-) “as a means of communication”, and (-leukin) “deriving from the fact that many of these proteins are produced by leukocytes and act on leukocytes”. The term interleukin was coined by Dr. Paetkau, University of Victoria. Being non-structural proteins, biological properties were and still are the gold standards for defining a cytokine. The interleukin nomenclature was invented to deal with the issue of multiple biological properties of cytokines. At the time of naming these molecules with an interleukin number, primary amino acid sequences of the active molecules were not known. But the nomenclature did nothing to resolve the broader issue of multiple biological properties ascribed to a single molecule.3
Classification of Cytokines
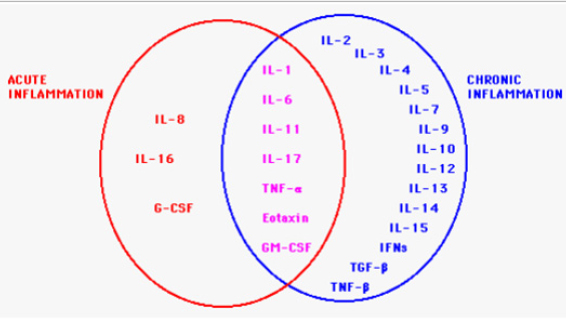
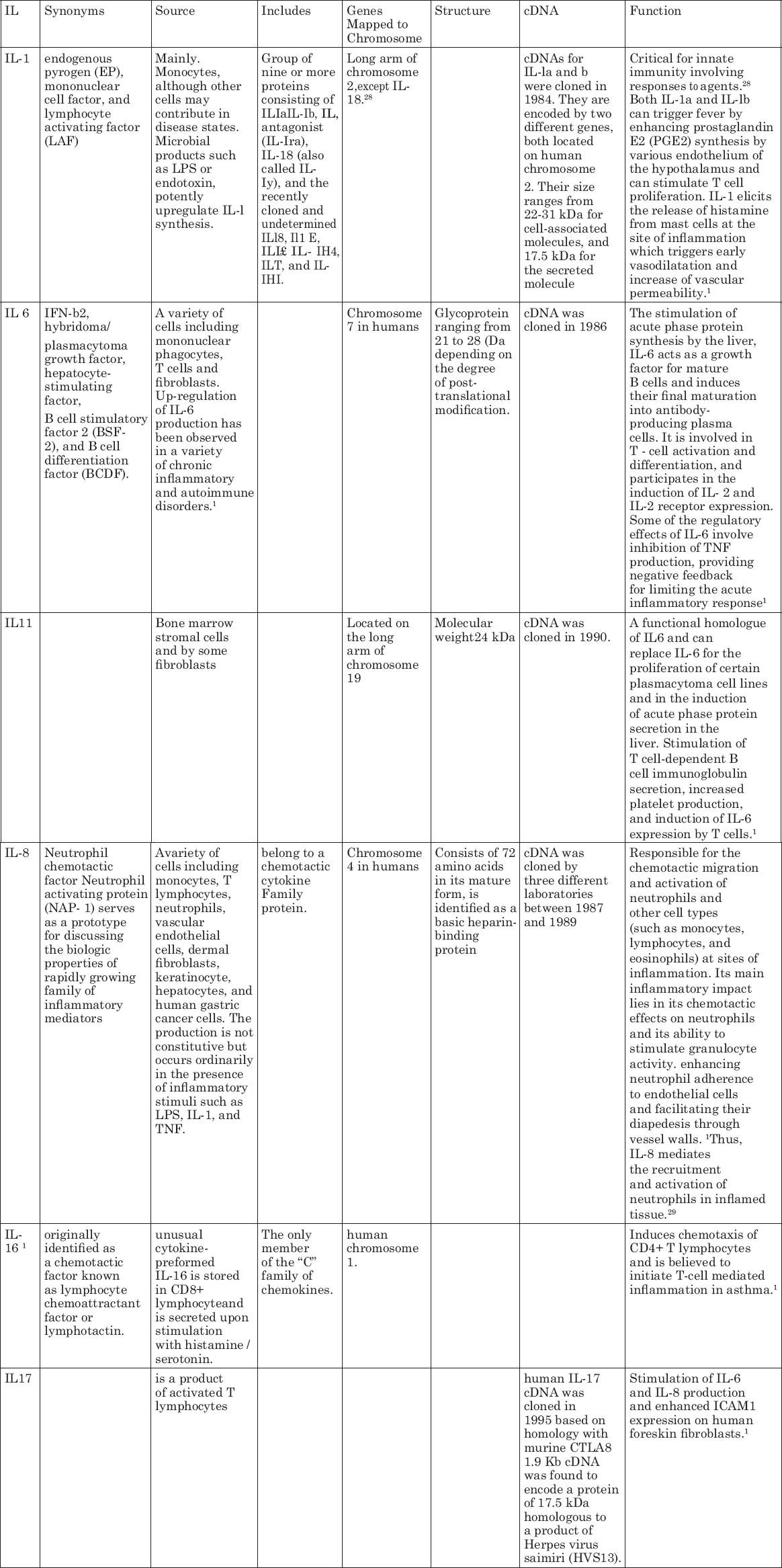
The local host response to the oral pathogens capable of causing periodontal disease includes the recruitment of leukocytes and the subsequent release of inflammatory mediators and cytokines, which appear to play crucial roles in the pathogenesis of periodontal diseases.2, 4 Cytokines are generally classified by their ability promote or inhibit inflammatory responses.5 The classification of cytokines is shown in. An inflammatory cytokine is defined as a cytokine which is induced during the course of an inflammatory response and is closely associated with its onset and/or progression. Thus far, IL-la, IL- 113, IL-6, 1L-8, and TNI-7-7 are generally classified as inflammatory cytokines.5
INTERLEUKINS INVOLVED IN INFLAMMATION
|
Click here to view |
CYTOKINES V/S CHEMOKINES
The term chemokines, a short form of ’chemotactic cytokines’, was coined in 1992. All the 50 or so human chemokines that were discovered over the years have chemo-tactic activity. They constitute a large family of mediators of inflammation and immunity with similarity to cytokines, but also some clear differences. Like cytokines the chemokines are secretory proteins produced by leucocytes and tissues cells either constitutively or after induction, and exert their effects locally in paracrine or autocrine fashion.
Interleukin Expression in Gingival and Periodontal Health
Tissue homeostasis represents a delicate balance between anabolic and catabolic activities. The regulations of migration, proliferation and differentiation of resident cells and of the production of tissue matrix in a healthy state are major aspects of periodontal tissue homeostasis. There is abundant evidence that myriad cytokines are involved in the maintenance of periodontal tissue turnover or integrity.2
Epithelium
The epithelium plays an active role in the pathogenesis of inflammation The gingival epithelium consists of keratinocytes, Langerhans cells, T-cells, Merckel cells and melanocytes.3 Keratinocytes, when challenged, with bacterial infection, express a large variety of cytokines and growth factors including interleukin-1 alpha (IL-1a), interleukin-8 (IL-8), tumor necrosis factor-alpha (TNF-a) and platelet-derived growth factor(PDGF). However, it is unknown whether cytokines and growth factors expressed by gingival epithelium are released in amounts sufficient to regulate remodeling in connective tissues of the periodontium.6
Connective tissue (fibroblast)
The dominant cell types are fibroblasts in the gingiva and fibroblast-like cells (called periodontal ligament cells) in the periodontal ligament. These cells express a variety of membrane and intracellular receptors, making the cells sensitive to regulate by many physiological and pathological, paracrine and endocrine signaling molecules.6 During inflammation, resident gingival fibroblasts are triggered by cytokines( released by macrophages) to enhance their synthesis of cytokines. IL-1 is the most potent regulator of extracellular matrix turnover by enhancing the expression of several matrix metalloproteinase. Interleukin-1 beta (IL-1b) and TNF-a stimulate the expression and release of interleukin-6 (IL-6), leukemia inhibitory factor and Interleukin-11 (IL- 11) in human gingival fibroblasts.8
Interleukins play a major role in initiation and progression of inflammatory process. However, a variety of different interleukins are involved in acute inflammation. These are summarized in Table 2

|
Table 1: Time in days taken for decalcification by manual and hot air oven technique
Click here to view |
|
Table 2: Soft tissue integrity by manual and hot air oven technique
Click here to view |
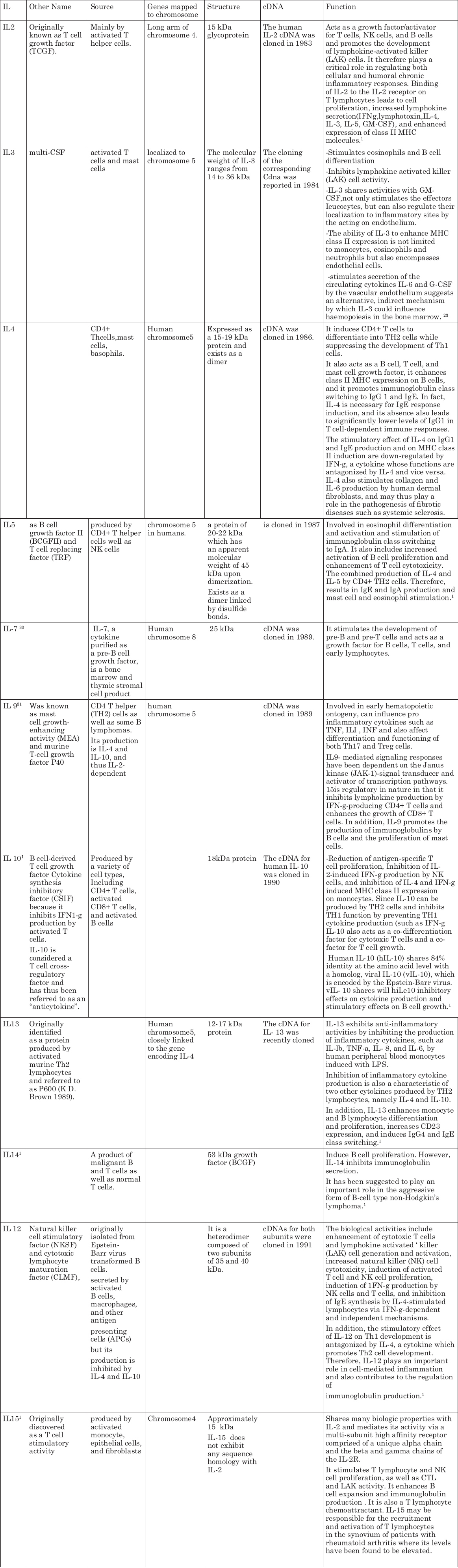
Interleukins Involved in Chronic Inflammation
Chronic inflammation may develop following acute inflammation and may last for weeks or months, and in some instances for years.
The detailed description of interleukins involved in Chronic Inflammation is shown in Table 4.

|
Table 3: Staining characteristics by manual and hot air oven technique
Click here to view |
|
Table 4: Cumulative scores of the decalcifying agents based on various parameters.
Click here to view |
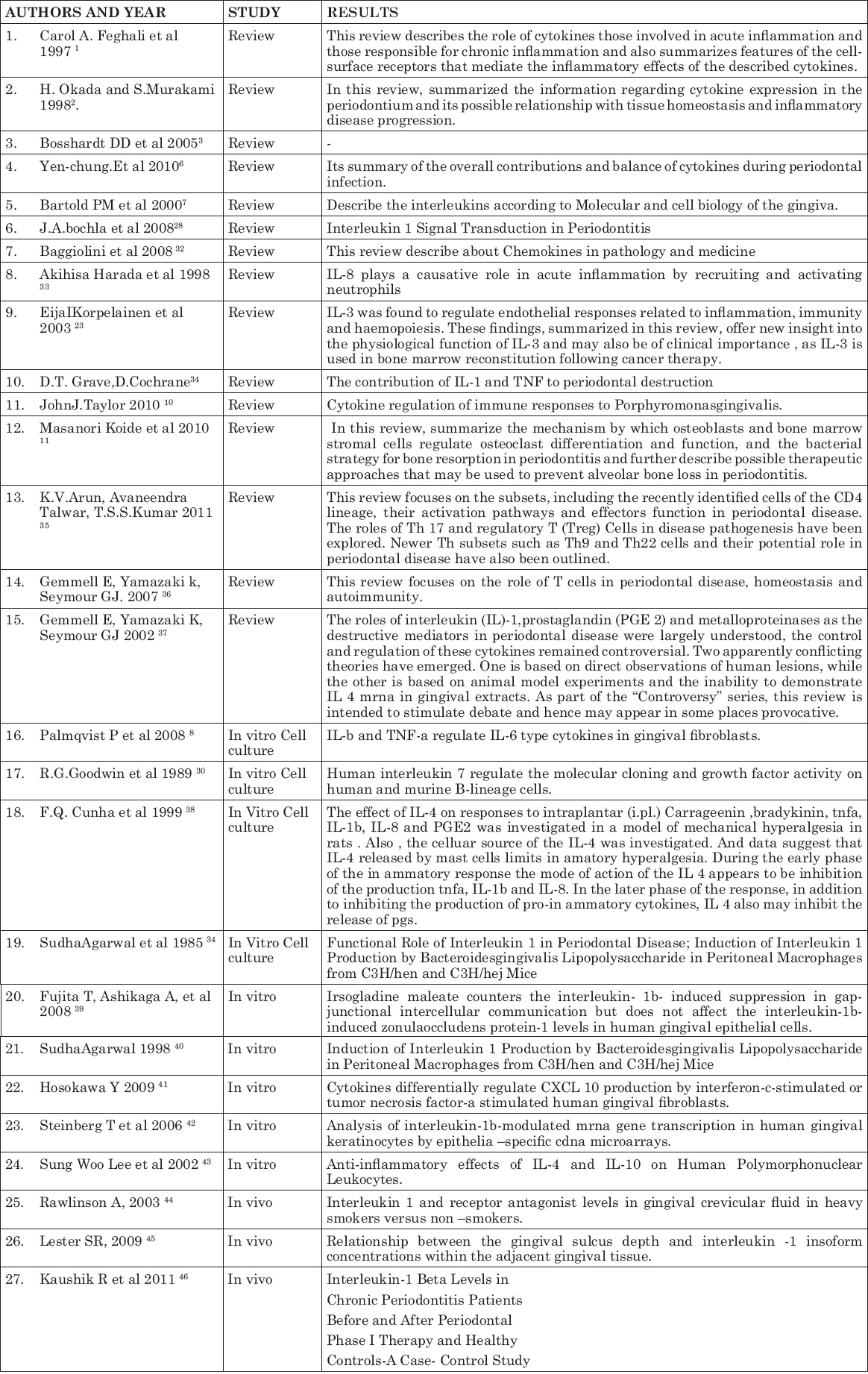
EVIDENCE
A variety of studies have been conducted to elicit the function and structure of interleukins.These are summarized in Table 5.
|
Table 5: Review of Literature
Click here to view |
Role of Interleukins in Pathogensis of Gingival Diseases
Phenytoin drug is used for treatment of epilepsy.It reacts with phenotypically distinct subpopulation of gingival fibroblast and cause an increase in protein synthesis and cell proliferation rate. IL1 and 6 found in higher levels in gingival crevicular fluid in phenytoin induced gingival over growth. It is suggested that this interleukin play indirect role in complex mechanism of phenytoin induced gingival over growth.9
Role of Interleukins in Pathogenesis of Periodontal Diseases
IL- I is known to stimulate the proliferation of keratinocytes, fibroblasts, and endothelial cells in an autocrine or paracrine fashion, and to enhance fibroblast synthesis of type I procollagen, collagenase, hyaluronate, fibronectin, and prostaglandin E2. IL-I is, therefore, a critical component in the homeostasis of periodontal tissues.6, 10 These mediators may be responsible for effecting connective tissue destruction, leading to loss of attachment. IL-1a, IL 1b, and TNF-a stimulate bone resorption and inhibit bone formation. It synergizes the bone-resorptive actions of TNF-alpha, induces the production of matrix metalloproteinase (MMPs), gives rise to an elevated level of procollagenase in both gingival fibroblasts and periodontal ligament (PDL) cells.6 No significant change in tissue inhibitors of metalloproteinase (TIMP) synthesis and mRNA was observed after treatment of gingival fibroblasts and PDL cells with IL- I b. In addition, IL-1 stimulates plasminogen activator in gingival fibroblasts, resulting in the generation of plasmin which is a putative, naturally occurring, activator of several matrix metalloproteinase.

|
Figure 2: Immune responses induced by interleukin-1, diacyllipopeptide and lipopolysaccharide induce the production of proinfiammatory factors in the target cells.
Click here to view |
Interleukin-1, diacyllipopeptide and lipopolysaccharide are recognized by interleukin-1 receptor (IL- 1 R), a complex of TLR2 and TLR6, and TLR4, respectively. CD14 is a membrane- anchored glycoprotein that aids the binding of lipopolysaccharide and TLR4. IL-1R and the TLRs possess a common TIR domain. Through their TIR domains, IL-1R and the TLRs activate MyD88 as a common signaling molecule. TRAF6 is a signaling molecule downstream of MyD88. Thus, interleukin- 1 and diacyllipopeptide activate the MyD8S / TRAF6 pathway to induce biological responses. In contrast, TLR4 has two signaling pathways: the MyD88 / TRAF6 pathway and the TRAM / TRIF pathway. The TRAM / TRIF pathway plays an essential role in interferon-b production. In macrophages, both the MyD88/TRAF6 and TRAM TRIF pathways are required for lipopolysaccharide-induced biological actions such as interleukin-6 production. Lipopolysaccharide isolated from P. gingivalis was shown to use both TLR4 and a complex of TLR2 plus TLR1 or TLR6 to induce biological responses, PGE2, prostaglandin E2; IL, interleukin; LPS, lipopolysaccharide; MR. Toil-like receptor; TNFa, tumor necrosis factor a; TRAF6, TNF receptor associated factor 6 MyD88, myeloid differentiation factor 88; TIR domain, Toll I IL-1R domain; TRW, TIR domain-containing adaptor-inducing interferon- b; TRAM, TRIF-related adaptor molecule11
IL 12 is regarded as a pro-inflammatory cytokine with immunoregulatory function, it may be greatly involved in chronic periodontitis.IL-12 acts not only as an activator of macrophages in the inflammed tissue, increasing their phagocytic and bacteriocidal activity, but also increases the ability of macrophages to produce IL 12 in a powerful positive feedback loop . It acts as both as an inflammatory mediator and also initiate host immune response within the periodontal tissues.6It was also suggested that IL-6 may act as an autocrine and/or paracrine factor in bone resorption in pathologic states by stimulating the formation of osteoclasts and the activation of osteoclastic bone resorption.11 Locally secreted IL-8 induces neutrophil extravasation at the site of inflammation and that the numerous neutrophils present in the lamina propria and the epithelium of inflamed gingiva may be directed there by IL-8.11
Interleukins in Connective Tissue Destruction
An early event in pathogenesis of periodontal disease is dissolution of approximately 70% of gingival connective tissue. Collagen breakdown may occur by two pathways (intracellular and extracellular). ILI inhibit the intracellular pathway while stimulating extracellular route, induces the production of MMPs and elevated level of procollagenase in both gingival fibroblasts and periodontal ligament, stimulates the plasminogen activator in gingival fibroblast resulting in generation of plasmin which is naturally occurring activator for MMP .
Interleukins in Bone Destruction
Hausmann speculated that periodontal bone loss was multifactorial, “involving a series of interactions between agent in plaque and mediators in periodontal tissue.12 Once “critical level of proinflammatory cytokine production is reached, a physiologic response become pathologic. If the infiammation occurs predominantly in the cementum, it will result in loss of attachment.If occurs near alveolar bone, bone loss occurs. If the inflammatory front does not progress far from the epithelium, the resulting lesion restricted to gingivitis.
PMN’s and monocyte of innate immune response produce ILI and TNF a that produces bone resorption. IL6 causes bone resorption in pathological state by stimulating the formation of osteoclast and activation of osteoclastic resorption. 1L8 is potent chemotatic for leukocyte and induces extravasation of neutrophils at the site of inflammation. These neutrophils contribute to local tissue destruction and bone resorption of periodontal tissue. 1L17 which shown to stimulate endothelial cell, fibroblastic cell to produce IL6, IL8 and PGE2 which are good activator for RANKL production by osteoblast and thus influence on osteoclastic bone resorption.
Interleukins in Chronic Periodontitis
Chronic periodontitis is an inflammatory response in the periodontal tissues. Chronic periodontitis in adults typically follows a cyclical course, with some forms remaining stable over many years and other forms progressing with subsequent tooth loss despite extensive treatment.13 The initial immune response in chronic periodontitis occurs following colonization of the gingival sulcus by periodontopathic bacteria. The presence of the bacteria induces the production of cytokines and chemokines by the gingival epithelium. This results in the expression of adhesion molecules, increased permeability of gingival capillaries and chemotaxis of polymorphonuclear neutrophils through the junctional epithelium and into the gingival sulcus. The specific cytokines and chemokines produced by this initial response lead to a perivascular T-cell / macrophage dominated inflammatory infiltrate in the connective tissues. If this cell-mediated immune response does not control the bacterial challenge, progression to a B-cell /plasma-cell lesion occurs. The antibodies subsequently produced may be protective and control the infection, or may be non-protective with resultant connective tissue destruction and bone loss.14 The early / stable lesion of chronic periodontitis is dominated by macrophages and T- cells, suggesting that Th1 cytokines are important in the development of this response, while the advanced/progressive lesion of chronic periodontitis, which is characterized by B-cells and plasma cells, is dependent upon Th2 cytokines.15 Thl cytokines include interleukin-2 and interferon-gamma and promote cell-mediated immunity, while the Th2 cytokine, interleukin-4, suppresses cell-mediated responses and enhances humoral immunity. A reduced Th l response has been shown in chronic periodontitis, where peripheral blood mononuclear cells obtained from patients with chronic periodontitis and then stimulated with mitogens , Porphyromonas gingivalis and Fusobacteriumnucleatum showed lower levels of Th1 cytokines(IL2,interferon gamma).Additionally, increased levels of Th2 cytokines (IL-4, IL-5, IL-6, IL-9, IL-10, and IL- 13) have been reported in GCF, gingival tissue15 and peripheral blood of patients with chronic periodontitis.16
The role of interleukin-10 in human chronic infections is both complex and critical. It has been implicated in the pathogenesis of chronic periodontitis , is critical in controlling the balance between Thl cells and Th2 cells in chronic periodontitis, whereby an excess of interleukin-10 may shift the balance in favor of a Th2 response and progressive disease, whereas its shortage leads to increased interleukin-1 production and increased tissue destruction.17 By contrast, high levels of IL 10 may even inhibit B-cell activation and proliferation, hence further illustrating its complex role. Low levels of IL-10 have been demonstrated in chronic periodontitis lesions compared with gingivitis, which may allow continued polyclonal B- cell activation to occur.18
Th17 cells are characterized by the production of interleukin-17. Th17 cell development depend upon the presence of interleukin-23 (a monocyte product) and also IL6 and TGF-b. Interleukin-17 expression is higher in chronic periodontitis tissues than in healthy tissues, along with IL-1b andTNF- a.19 It induces the production of pro-MMP-1 and MMP-3 by gingival fibroblasts. In contrast, interleukin-17 receptor knockout mice showed increased P. gingivalis-induced periodontal bone loss, suggesting its possible protective role ingingivalis-induced tissue destruction.20-22.
IL- 1 levels were elevated in GCF at periodontitis sites and that marked reductions of total IL- 1 levels were observed following effective treatment. They also commented that IL-b was detected more frequently than IL-lex in GCF from untreated patients with periodontitis.21
Interleukins in Refractory Periodontitis
Reinhardt and colleagues (1993) reported that elevated levels of IL1a, IL-13, and IL-6 were detected in the GCF of patients with refractory periodontitis. A possible correlation among bleeding index, probing depth, and the IL-6 levels of the crevicular fluid has also been demonstrated.21
Interleukins in Aggressive Periodontitis
B-cell/plasma-cell nature of the aggressive periodontitis lesion makes it likely obe Th2- mediated lesion. It has been shown that Th17 cells can be converted to Thl cells or Th2 cells under the influence of interleukin-12 or interleukm-4 respectively, while CD4+, CD25+,forkhead box P3 (Foxp3+) regulatory T-cells can be converted to an interleukin-17-producing cell when co-cultured with dendritic cells selectively activated via dectin-1. These latter findings highlight the complex regulatory networks that are probably operating in both chronic and aggressive peniodontitis.23
IL-8 is a chemoattractant for neutrophils expressing the receptor CXCR1. Enhanced accumulation of neutrophils in the pocket epithelium and adjacent connective tissue of patients with chronic periodontitis and with generalized aggressive periodontitis (GAP)s was associated with the upregulation of IL8, intercellular adhesion molecule-1, IL-1b and TNF—a expression, which related to the severity and activity of generalized aggressive periodontitis.24 Anne Havemose-Poulsen in 2005 compared Cytokine Profiles in Peripheral Blood and Whole Blood Cell Cultures Associated With Aggressive Periodontitis, Juvenile idiopathic Arthritis, and Rheumatoid Arthritis, found that two anti-inflammatory cytokines,IL10 and IL1Ra were significantly elevated in GAP patients and patients with aggressive periodontitis and type of arthritis presented with similar components of blood cytokine profiles distinguishing them from individuals free of disease. Interestingly, it has recently been shown that infection of human macrophages with A. actinomycetemcomitans (Aa), a bacterium associated with certain forms of aggressive periodontitis, results in the profound release of activeIL-1b, an effect considerably larger than that induced by LPSand not associated with enhanced secretion of interleukin-6 or TNF. The effect is mainly dependent on the leukotoxin from A. actinomycetemcomitans
Interleukin Polymorphisms and Periodontitis
The systemic immune response, genetic and environmental factors also affect the risk of developing periodontitis. In recent years, studies have demonstrated that periodontitis is associated with elevated levels of a variety of inflammatory biomarkers. Furthermore, genetic variants of some cytokines confer susceptibility to periodontitis.3 As it is accepted that the immune system plays an important role in the pathogenesis of periodontitis, most genes that are considered to be responsible for the development of periodontitis are also linked to the immune response. These include the genes that affect the expression of IL1, IL-6, TNF-a, and IL- 10, E-selectins, Fc-gamma receptor, CD 14, toll-like receptors, caspase recruitment domain 15 and vitamin D receptor.1 Polymorphisms arises as result of insertion and deletion in nucleotide sequence. Genotype polymorphisms have also been associated with disease diagnosis, severity and presence of sub- gingival bacteria. IL8 and IL6 investigated for the relationship between periodontopathic bacteria (Aa &Pg) and bleeding on probing which shows that association is found in both aggressive and severe form of chronic periodontitis.
IL-1 Gene Polymorphism
IL-1 gene cluster is located on chromosome 2. The first study that reported polymorphism for IL- 1 gene in relation to periodontitis was presented by Korman et al, in Caucasians. He concluded that IL- 1 composite genotype could be considered a putative severity factor for periodontitis in Caucasians. Sensitivity and specificity of IL-1 “Genotype positive” model was depicted by Kornman et al, 1997.1 Anne Havemose - Poulsen et al. demonstrate that in localized aggressive periodontitis patients, allele 2 of IL - 1 RN VNTR(variable no. of tandem repeats) was associated with significantly higher levels of IL -1a, 6, 10 and TNF - a, whereas allele 2 of IL - 1p +3954 was associated with significantly lower levels of the same cytokine.
IL-4 Gene Polymorphism
IL -4- polymorphism was at the promoter sequence-590 C/T, -33C/T and intron 3. VNTR of IL4 acted in a cooperative fashion andresulted in high production of IL 4. In 2008, Stefan Reichert et al studied the expression or IL-12 R p2 molecule in a crucial regulatory factor in the T helper type differentiation of T cells. They found that single nucleotide polymorphism of the flanking region of IL -12RB2 leads to a very weak cellular immune response. They reported that the frequencies of variant alleles of IL 12 RB2 were significantly higher in aggressive periodontitis patients.
IL-6 Gene Polymorphisms
Shao et al 2009, in the meta-analysis indicate that the IL-6 ,-174 G allele could not modify the risk of chronic periodontitis, but increased risk of aggressive periodontitis. And -572 C/G polymorphism is associated with the pathogenesis of periodontitis, as it predisposes to either chronic or aggressive periodontitis.
IL-10 Gene Polymorphisms
IL-10 gene is located on chromosome 1, in a cluster with closely related IL-genes IL-19, - 24. IL- 10 has an inhibitory effect on IL-1a, IL-1b,TNF-a, IL-6,8 and 12. Functional disturbances in IL-10 due to genetic polymorphisms could be detrimental to host tissue and linked to periodontal disease susceptibility.
Implant Failure And Interleukin Polymorphism
Regarding the timing of implant failure, it can be classified as early when osseointegration fails to occur, or late when the achieved osseointegration is lost after a period of function. Infection, overheating and impaired healing are the main factors associated with early failure of dental implants. Of these, surgical trauma, a consequence of implant insertion, initiates a local inflammatory response that includes the release and activation of a variety of cytokines and growth factors. This local factor production determines the quality of bone formation or the formation of fibrosis. Increased levels of bone resorptive interleukins, such as IL-1, might stimulate an excessive inflammatory response, affecting osseointegration success.
A few studies have analyzed the relationship between interleukin-1 genepolymorphisms and implant failure. Wilson & Nunn (1999) were the first to study the relationship between implant loss and the interleukin-1 composite genotype reported by Kornmanet at (1997) [allele Tat interleukin- IA (889) and at interleukin-1B [p3953) loci]. Their analysis failed to provide a positive correlation, but these results might have been influenced by variables, such smoking and the existence of late and early failure implants in the same sample. Rogers et al. (2002) also found no association between the same. Campos et al 2004 also showed that polymorphism in the interleukin-1 RN (intron 2), interleukin- 1B (511, p3953) and interleukin-1A (889) genes were not associated with early implant failure in a nonsmoking Brazilian population.
Interleukins as Diagnostic Marker
The biochemical assessment of periodontal disease can be accomplished using several approaches. The most practical and least- invasive,involves analysis of biologic fluids that are derived from the periodontal tissues or contain specific mediators that are present as a result of periodontal disease. The biologic fluids that have been studied to understand the nature of destructive periodontitis and to identify potential diagnostic markers of active disease include serum (blood), gingival fluid, and saliva.
Blood
Studies of serum antibody levels to periodontal bacteria were among earliest investigations demonstrating that a humoral immune response occurs in patients with periodontitis. More recent studies have demonstrated that patients with periodontitis have elevated antibody titers to subgingival pathogens. The levels of inflammatory cytokines (ie, IL-6) and general markersof inflammation (ie, C-reactive protein) have been shown to be elevated in the blood of patients with periodontitis. Nevertheless, serum markers of periodontitits, or of inflammation, are not currently used as diagnostic tests for periodontitis.25
Gingival Crevicular Fluid
GCF is a serum transudate, or more commonly inflammatory exudates, that emanates from the gingival crevice and can be collected from the crevice orifice. GCF has been analysed for diagnostic purposes. Its constituents are derived from a variety of sources including host as well as from microorganisms in the subgingival and supragingival plaque. The collection and analysis of GCF samples provides a non-invasive means to assess the pathophysiological status of the periodontium in a site-specific manner. According to Armitage (2004), more than 65 GCF constituents have been evaluated as potential diagnostic markers of periodontal disease progression. These markers can be divided into three groups: host-derived enzymes and their inhibitors, inflammatory mediators and host-response modifiers, and byproducts of tissue breakdown. The inflammatory cytokines in particular IL-1b, may play an integral role in the etiology of periodontal disease. Lieu et al (1996) demonstrated that with an increase in gingival index and probing, there was a corresponding increase in IL-1b in both the gingival tissue and GCF. Engebretson et al through a longitudinal study suggested that GCF IL-1b expression is genetically influenced and not solely a result of local clinical parameters. Also, a GCF level of 1L8 was found to be higher in periodontal diseases and was influenced by local IL1 beta activities .26
Interleukins as Anti-Inflammatory and Antiresorptive Therapy
As inflammatory cytokines are involved in inflammatory diseases associated with bone loss and have therefore become logical targets for the development of therapeutic agents. One of the first cytokines to be targeted was IL-1 as a result of its key regulatory role in bone resorption in diseases such as rheumatoid arthritis and periodontitis. In addition, agents targeting IL-3,6,15,12 and 23 have been studied. These anti-cytokine agents provide new opportunities to modulate host responses in inflammatory diseases. In particular, most seem to influence the secondary effects of cytokines on RANKL expression and therefore may not influence osteoclast-mediated bone resorption directly. Future efforts in this area, to ensure more effective control of pathologic bone resorption should try to target those cytokines that directly influence osteoclast formation and function. Surprisingly few studies have investigated the effect of interleukin antagonists on periodontitis. One study investigating inflammation and tissue loss in a nonhuman primate model of periodontitis using human soluble interleukin-1 receptor type 1 as an inhibitor of IL-1 reported that the inhibition of IL-1 has a significant effect on the reduction of inflammation, connective tissue attachment loss and bone resorption .Given the emerging use of these agents as anti-inflammatory and anti-resorptive agents, further investigations in experimental models of periodontitis are arranted.27
CONCLUSION
Interleukins are key modulators of inflammation. They participate in acute and chronic inflammation in a complex network of interactions. Several cytokines exhibit some redundancy in function and share overlapping properties and structure.Theseplay an important role in a number of different physiologic processes, but if expressed inappropriately, they also induce pathology. Under pathologic conditions such as those that occur in periodontal disease, the balance between pro- and anti-inflammation is directed towards proinflammatory activity .In periodontal tissue destruction three proinflammatory cytokines, IL-1, IL-6, and TNF-a, appear to have a central role.
Better understanding of the pathways regulated by interleukins will allow the identification and/or development of agents for improved modulation of the inflammatory response for the treatment of periodontitis autoimmune, infectious, and neoplastic diseases.
