INTRODUCTION
Periodontitis is a complex disease in which disease expression involves intricate interactions of the biofilm with the host immuno inflammatory response and subsequent alterations in bone and connective tissue homeostasis. A model of the pathogenesis of periodontitis based on systems biology approaches should allow investigators to better communicate the interrelatedness of various biologic components involved in the initiation and resolution of disease.
Concepts of the pathogenesis of periodontal disease

|
Figure 1: Early linear model depicting the principal etiologic role for bacteria in the initiation and progression of periodontal disease.
Click here to view |
|
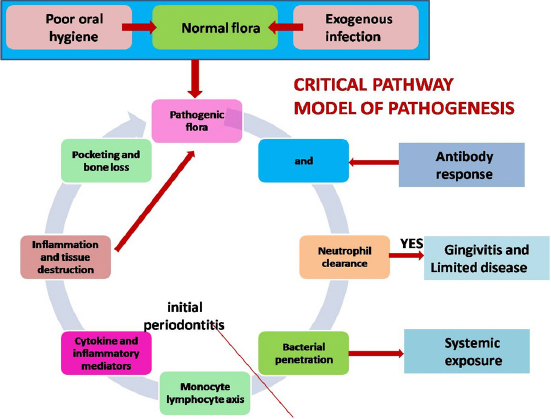
Figure 2: Circa 1980s model (Ivanyi L , Lehner T , 1980 ) emphasizing a central role for the host immuno-inflammatory response in the clinical development and progression of periodontal disease.
Click here to view |
The extensive research through the mid-1980s led to critical refinements in the pathogenesis concept.In most of the models of the late 1980s; specific bacteria initiated the disease process by activating host responses, which were protective and destructive. The actual destruction of connective tissue and bone resulted primarily from activated tissue mechanisms, such as matrix metalloproteinases, interleukin-1, and prostaglandins.10
|
Figure 3: Critical pathway model (Offenbacher, 1996)
Click here to view |
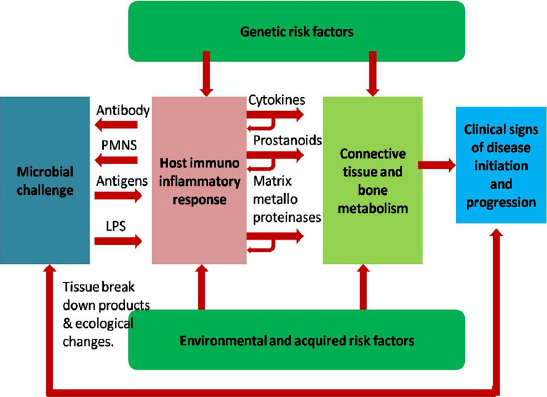
To add further complexity to the earlier conceptual models, there was a growing appreciation during this period which highlighted the genetic variations in the development and severity of periodontal disease which accounted for 30% to 60% of variability. Genetic differences among individuals seemed to be a significant determinant of risk for periodontal disease and, most importantly, there were gene variations that altered host responses and modified the clinical severity of disease.12 With new knowledge of the various factors contributing to periodontal disease, the clinical phenotype is not simply the microbial challenge translated by a standard host response but also smoking and diabetes were shown to be powerful determinants of disease severity.13, 14 This has led to raise several questions like
• Does periodontitis affects all individuals uniformly?
• Do progression is continuous & linear throughout life?
• Do disease severity is directly correlated to plaque levels?
|
Figure 4: Non- linear model, 1997
Click here to view |
Although many of the concepts presented in the 1997 non-linear model of periodontal disease remain relevant today, there have been advances in knowledge about periodontal disease that may alter our models of pathogenesis.
During the same period of time, there were substantial advances in knowledge about chronic diseases in general that have influenced our thinking about the pathogenesis of periodontitis. First, inflammatory mechanisms were recognized as being common to many chronic diseases, such as cardiovascular disease. Second, periodontitis and other chronic diseases were acknowledged as ’’complex’’ in character.Complex biologic traits, have molecular networks that display emergent properties as a result of contributions from genetic and environmental factors. Third, although the biology is complex, the integrated behavior of the entire system can be studied using new simulation tools. The fourth factor- complex diseases that may be applicable to models of periodontal pathogenesis involves the roles of environmental factors.
|
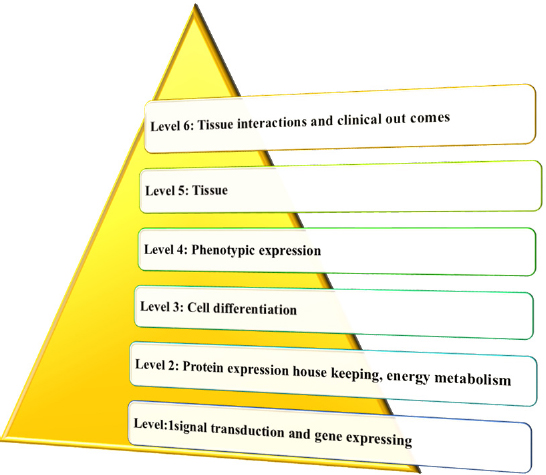
Figure 5: Multilevel hierarchal model
Click here to view |
Building a systems biology model of periodontitis presents substantial requirements and challenges, but investigators have started to provide data on the entities and gene and protein expressions associated with certain components of the periodontal model. This model involves bacterial components, environmental factors such as smoking and diabetes.18

|
Figure 6: Biologic systems model
Click here to view |
This provides a frame work for viewing the contributions and relative importance of all components that contribute to the clinical presentation of the periodontal disease and individual response, including cytokines and lipid mediators, produced by the host, as well as alterations in bone and connective tissue, can be clearly characterized by a specific pattern of gene, protein, and metabolite expression. The expressed proteins and metabolites provide feedback on the system to regulate the host response and bone and connective tissue, while helping to control the bacterial challenge.
CONCLUSION
Over the past 50 years, a number of conceptual models describing the pathogenesis of periodontal disease have been presented based on existing knowledge at the time. The more recently explored biologic systems approach to modeling holds promise for revolutionizing conceptual models of the past by providing a comprehensive view of the disease process as a complex regulatory network. Within this framework, discrete modules of genetic, environmental, and other modifying factors would define a specific expression pattern that represents the shift from health to disease.
