INTRODUCTION
Lip lesions can be manifestations of systemic diseases, a localized expression of dermatologic diseases or a localized condition of the lips.1 Cheilitis is classified into various types: angular cheilitis, actinic cheilitis, contact cheilitis, plasma cell cheilitis, cheilitis gland-ularis, cheilitis granulomatosa, exfoliative cheilitis and factitious cheilitis.2 Thorough clinical history, basic laboratory tests and histopathologic evaluation are required to exclude other diseases. Exfoliative cheilitis is a rare disease which affects the vermilion border of the lips. It is characterized by unremitting production and desquamation of thick scales of keratin. 1, 3 Symptoms may include sensitivity and burning of the lips, and affected patients may avoid socializing due to the unsightly appearance of the lips.4 Although the cause is unknown, EC has been associated with underlying stress and anxiety as well as parafunctional/factitial activities including lip licking and chewing.5, 6
CASE REPORT
A 28 year old female patient reported to our post graduate Department of Oral Medicine and Radiology with chief compliant of crustation of lips for the past 3 years (Figure 1) associated with periods of exacrabations and remissions. According to patient crustations were preceeded by diffuse swelling and itching sensation of lips followed by progressive thickening of superficial layers of lips and crustations which persists for few days and then peels off revealing underlying thin mucosa which often used to be raw.

|
Figure 1: Clinical picture showing pretreatment condition of lip with marked crustation.
Click here to view |
Patient had consulted many dermatologists for the same illness and was subjected to many investigations to rule out Bacterial, Viral and rheumatological diseases. Investigations like HBsAg, anti-Hcv, Hiv, EBV, CMV serology were done which were negative. Patient was also subjected to pathergy test, montoux test, test for brucellosis and sarcodosis which were all negative. Patient also visited rheumatology department where she was investigated for autoimmune disease. Rh factor, C-reactive protein, Anti Nuclear antibody, anti ds DNA levels were within normal limits. Finally patient was referred to the department of Oral Medicine and Radiology to rule out any oral foci of infection. After performing all base line investigations and under all aseptic precautions an incisional biopsy was performed (Figure 2) and specimen was sent for histopathological examination and fungal culture.

|
Figure 2: Site of incisional biopsy.
Click here to view |
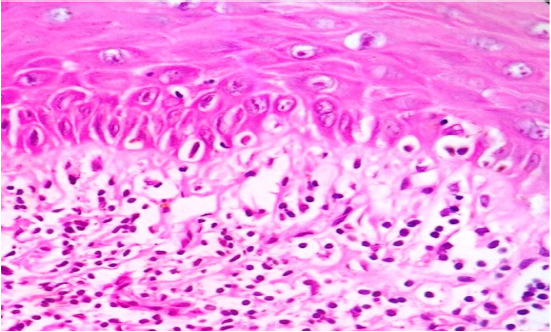
Histopathological examination showed marked hyperkeratosis and parakeratosis, mild inflammatory infiltrate, without any significant characteristic feature and (Figure 3).
|
Figure 3: H & E stained section showing non specific histopathological picture.
Click here to view |
Fungal culture was also negative. From clinical examination, history and biopsy report it was clear that all features were suggestive of exfoliative cheilitis. When the patient was asked about the habit of lip picking or licking, she admitted that she had the habit but she had left the habit because of this condition now. Patient was emotionally disturbed because of the unesthetic appearance so a psychiatric consultation was done and patient was put on clonazipam 0 .5mg at bed time meanwhile treatment of exfoliated cheilitis was commenced with local application of antikeratotic ointment 0.005% retinoic acid qid, Betamethasone 0.01% tid , euciren emollient cream with 10% urea and patient was advised to keep her lips always moist by using some lip baam in between and at the same time avoidance of lip licking was advised. A great improvement was seen after 15 days of treatment, upper lip was completely normal and great improvement was seen in lower lip. Crustations were resolved in middle portion, only small scales were present on lateral portion of lower lip (Figure 4 and 5). Same treatment regimen was continued and patient is on regular follow up however the condition has not completely resolved there are still periods of exacerbation.

|
Figure 4: Clinical picture showing post treatment condition of lips after 15 days.
Click here to view |

|
Figure 5: Clinical picture showing post treatment picture after 30 days.
Click here to view |
DISCUSSION
Less than 200 cases of EC have been reported in the lit-erature (51 cases in the English literature) and their di-agnosis was totally based on history and clinical feature.7, 8 Exfoliative cheilitis reportedly occurs more commonly in females.1, 9 The majority (62%) of patients affected were younger than 30 years of age, many of whom were younger than 20 years of age same is the case with this patient.7 Clinician’s knowledge of the clinical course of this disease is important for accurate diagnosis. Exfoliative cheilitis is an infrequently mentioned condition; details given about the course of this disease are inadequate. One of the leading hypotheses is that EC develops secondary to parafunctional activities, including lip licking and lip biting. Patients with psychologic conditions such as anxiety, depression, or obsessive compulsive disorder may have more persistent chronic parafunctional activities that can contribute to the development of EC.10 The present patient too was mentally disturbed however she had now left the habit of lip licking because of the pain and discomfort associated with even slight movement of lips and has lost weight because of loss of appetite and discomfort associated with normal functional activity of mouth. However, most patients treated with antidepressants showed improvement in, but no complete remission of the disease. In this case, patient’s condition improved when she was on antidepressants, but she too had no complete relief. Raede and others discussed the possibility of cheilocandidosis.5 It involves compromised immunity or the presence of other obvious predisposing factors that cause candidal infection of the lips. The authors achieved successful resolution of such lesions with antifungal therapy. However, for people who have no specific predisposing factors, such as our patient and others Candida could not be isolated from the lesion nor did the condi-tion respond to antifungal therapy.11 Fungal colonies have been reported on histologic examination, but these appear to be superficial and are likely secondary findings rather than being pathogenic, as is typical with intraoral factitial/ frictional keratosis.12 Oral sepsis has also been implicated as a cause of ex-foliative cheilitis as in this case too patient had a very poor oral hygiene because it was dif-ficult to maintain good oral hygiene.13 Her condition may be the result of multifactorial causes such as factitious habit, oral sepsis, associated with and aggravated by stress that resulted in clinical depression. Atopy, actinic damage, cheilitis granulomatosa, plasma cell cheilitis, contact dermatitis, discoid lupus erythematosus and neoplasia should be considered in the differential diagnosis of crusted and ulcerated lesions of the lip.14 Thorough clinical history, basic laboratory tests and histopathologic evaluation are required to exclude other diseases.
Histologically, exfoliative cheilitis is characterized by marked hyperkeratosis and parakeratosis without significant inflammation. This could be reactive hyperplasia of the epidermis due to repetitive trauma in the form of regular picking of the lips. Trauma may induce epidermal proliferation resulting in parakeratosis and hyperkeratosis.14 So biopsy is the gold standard for diagnosis of this condition along with history of clinical course of the disease. Exfoliative cheilitis may resolve spontaneously but if persistent, it is usually refractory to treatment and difficult to manage.3, 11 Previous studies for the most part have reported no benefit with antimicrobial agents (systemic and topical), corticosteroids (systemic and topical), petroleum jelly, sunscreen, and dietary supplements such as folic acid and iron.3, 4, 8, 9, 15 Systemic therapy with antidepressants including sertraline, fluvoxamine, diazepam, and amitriptyline led to at least partial improvement in all patients treated.371516 Because none of these were controlled studies, it is unclear to what extent the efficacy associated with antidepressant medications was due to modification of parafunctional habits or simply to the natural course of the condition. EC can be easily confused with other dermatologic conditions that affect the lip, such as allergic contact cheilitis and atopic cheilitis. These lip conditions present with erythema, dryness, scaling, and fissuring. The most common causes are cosmetic materials, metals (commonly nickel), and dental materials. These can be distinguished from EC by a positive history of contact with the allergen/hapten, positive allergy or patch testing, and substantial response to elimination of the allergen. In the present case there was no history of use of new creams, toothpaste or cosmetic items around the lips before the problem began more over pathergy test also was negative. Avoidance of lip sucking or biting and use of lip moisturizers has been the mainstay of therapy. Psychiatric evaluation is essential for diagnosing any emotional stress that can exacerbate lesions19? In this report, pre-scription of clonazepam 0.5 mg daily with antikeratotic cream Retinoic acid 0.005%, Betamethasone 0.01%, lip balm and Eucerin emollient cream (10% urea) together caused a significant improvement. Urea is produced naturally in the skin and causes moisture ab-sorption and helps to rehydration of dry and scaly skin. Furthermore, urea in the Eucerin emollient cream (10% urea) penetrates to the horny layer of skin and increases the skin’s capacity to absorb moisture. Eucerin covers skin surface as oil layer, which prevents water evapora-tion from this surface. Side effects of urea are skin irrita-tion such as burning, itching or erythema; however, in the present case there were no side effects. However these agents, combined with intensive counseling and psychotherapy have not yielded desired or satisfactory results. Therefore, besides the above mentioned agents various therapeutic modalities like cryosurgery, intralessional methotrexate injections have been tried in the past with variable outcomes. All of them were aimed at reducing excessive keratin and provides temporary and symptomatic relief. As the present patient had severe inconvenience and cosmetic disfigurement due to the disease, we tried local antikeratotic agent, local steroid and eucerin ointment to reduce excessive epidermal proliferation. In this patient, significant improvement in scaling and erythema was seen. As such, it is difficult to be certain whether patient responded because of the anti-inflammatory effect of the ointment or because the ointment or moisturizing agents were emollient and thus helped to keep the lips moist, protected the area from irritants, or increased the patients’ awareness of the habit, helping them to reduce trauma to the site This case highlights the fact that exfoliative cheilitis is secondary to compulsive lip licking and psychiatric consultation along with above mention treatment regime can be used as therapeutic option in severely affected patients.
CONCLUSION
Exfoliative cheilitis predominantly affects females under 30 years of age lower lip is affected more as compare to upper lip and typically follows a cyclic course characterized by normal or erythematous lips Given the scarcity of reports in the literature and the lack of a strong evidence base to guide therapy, management of EC will likely remain a challenge for clinicians and patients. Prospective multicenter trials are unlikely owing to the infrequent occurrence of EC. Larger case series from multiple centers would be helpful in understanding the natural course of EC and in identifying the most effective management strategies. No appropriate treatment has been identified for this condition because the cause remains unclear.
