INTRODUCTION
Orthodontist is no magician to bring the teeth into alignment without the support of the anatomy and the physiology underlying. However, the anatomy sometimes can constitute a limitation for the orthodontic tooth movement and the same has been explained by the ven-diagram of Envelop of discrepancy by Ackermann and Proffit which literally gives the bird’s eye view of the possibilities of tooth movement in all the dimensions.1
Sound knowledge of anatomy and the cellular biology is must for an orthodontist to diagnose and treat a case in a physiologically sound manner. Most of the earlier studies which dealt with the anatomical constraints have stressed the limitation to the orthodontic tooth movement.2-9 The possibilities of iatrogenic damage by the orthodontic treatment are high in case of the scanty alveolar bone thickness.
The well versed damage includes the gingival recession, the wash board appearance, fenestrations and dehiscence and the root resorption.10-16 The best way to address such problems is to prevent such problems from budging up. For so much so as to the prevention is better than cure, one has to know the alveolar bone anatomy in different malocclusions and growth pattern. With this as a background the present study was aimed to assess the alveolar bone thickness in the Indian adults who required orthodontic treatment.
MATERIALS AND METHODS
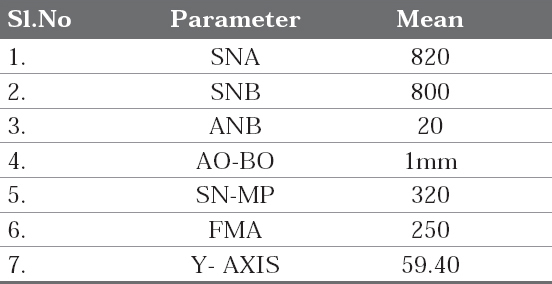
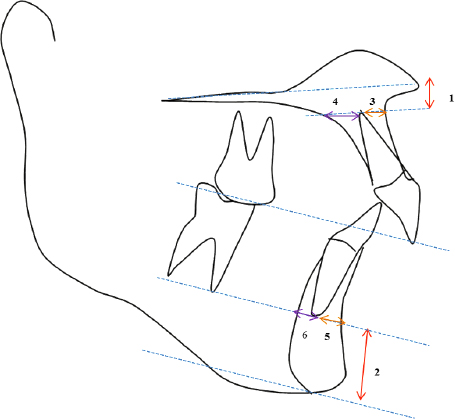
A cross sectional study was conducted in the department of orthodontics and dentofacial orthopedics. Ethical clearance for the study was obtained by the institutional ethical committee. The pretreatment lateral cephalograms of hundred adult patients were retrieved from the record section of the department. Age of the sample ranged from 18-35 years. All the lateral cephalograms were taken in the centric occlusion using the standard protocol in natural head position. The cephalograms were traced for the standard sagittal skeletal parameters (Table 1) and were grouped into class I, class II and class III categories. Each category was traced again for the standard vertical parameters (Table 1) and was regrouped into low, average and high angle class I, class II and class III cases respectively. Finally, the lateral cephalograms were traced for the anterior alveolar anatomy of the upper and lower jaw using the parameters suggested in the earlier study of similar kind by Handelman (1996)8 and the same is represented in figure 1.
|
Table 1: Sagittal and vertical parameters
Click here to view |
|
Figure 1: Measurements used for Measuring the Alveolar Width of Maxilla and Mandible
Click here to view |
UAH: bone superior to the upper incisors. Measured from the upper incisor root tip to the palatal plane
LAH: bone inferior to the lower incisors. Measured from the lower incisor root tip to the tangent to the lowest point on the symphysis which is parallel to the occlusal plane
UAAW: bone anterior to the upper incisor. Measured from the upper root apex to the labial cortical plate along the plane parallel to the palatal plane
UPAW: bone posterior to the upper incisor. Measured from the upper root apex to the palatal cortical plate along the plane parallel to the palatal plane
LAAW: bone anterior to the lower incisors. Measured from the lower incisor root tip to the labial cortical plate along the plane drawn through the lower incisor apex parallel to the occlusal plane.
LPAW: bone posterior to the lower incisors. Measured from the lower incisor root tip to the labial cortical plate along the plane drawn through the lower incisor apex parallel to the occlusal plane.
The collected data was tabulated and was subjected to descriptive statistical analysis using SPSS 15. One way ANOVA was applied to check the difference of alveolar bone morphology between different groups of malocclusions and the different growth patterns.
RESULTS
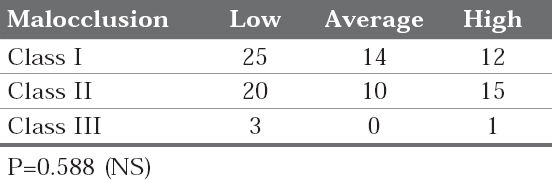
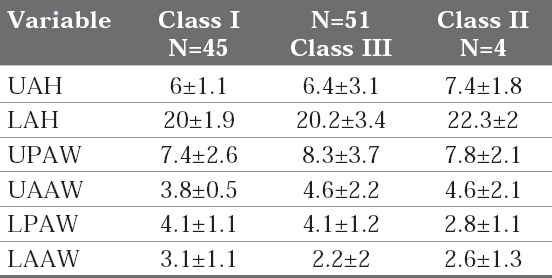
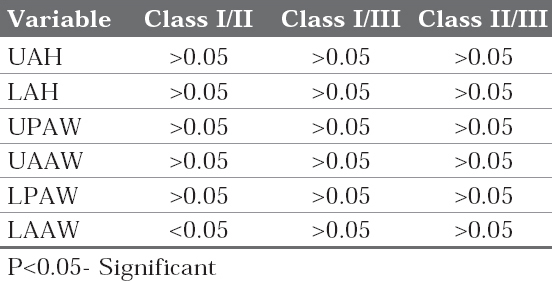
Table 2 represents the sample division into class I, II and III with respective mandibular divergence. Comparatively class III malocclusion sample was less. The alveolar bone measurements are depicted in table 3A for different malocclusion groups and the p-value for the malocclusion groups is shown in table 3B. The results show that there existed significant difference between class I and class II malocclusion for the lower posterior alveolar bone thickness.
|
Table 2: Number of subjects in nine subgroups defined by Angle classification and mandibular divergence SN-MP (N=100)
Click here to view |
|
Table 3A: Width and Height of anterior alveolus for different malocclusion groups.
Click here to view |
|
Table 3B: P-value for the measured alveolar bone thickness for different malocclusions
Click here to view |
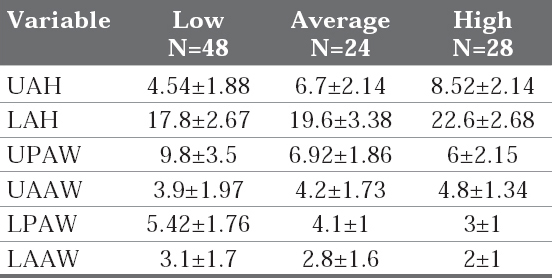
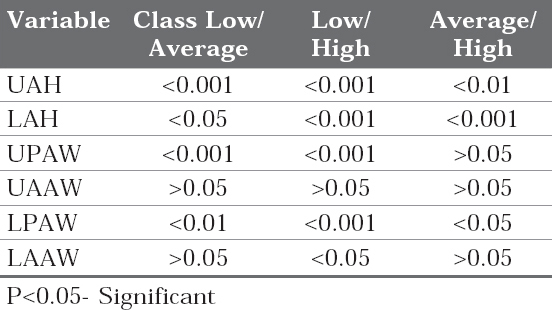
The table 4A and 4B represent the different alveolar bone measurements for the different mandibular divergence groups and their p-value respectively. There existed a highly significant difference for the height of the upper alveolar bone and the upper posterior alveolar bone thickness between the low and average mandibular divergence groups. Whereas, for the low and high mandibular divergence groups, highly significant difference (p<0.001) was found for the upper and lower alveolar bone height; the upper and lower posterior alveolar bone thickness. For the average and high mandibular divergence group the highly significant difference was noted only for lower alveolar bone height.
|
Table 4A: Width and height of anterior alveolus for different mandibular divergence groups
Click here to view |
|
Table 4B: P-value for the measured alveolar bone thickness in different mandibular divergence groups
Click here to view |
DISCUSSION
The main objective of the study was to explore the natural morphological constraints for the effective orthodontic tooth movement. In the earlier literature same constraints were termed as “orthodontic walls” and the term seems to be rightly coined for the way we orthodontist are bound to these constraints.8
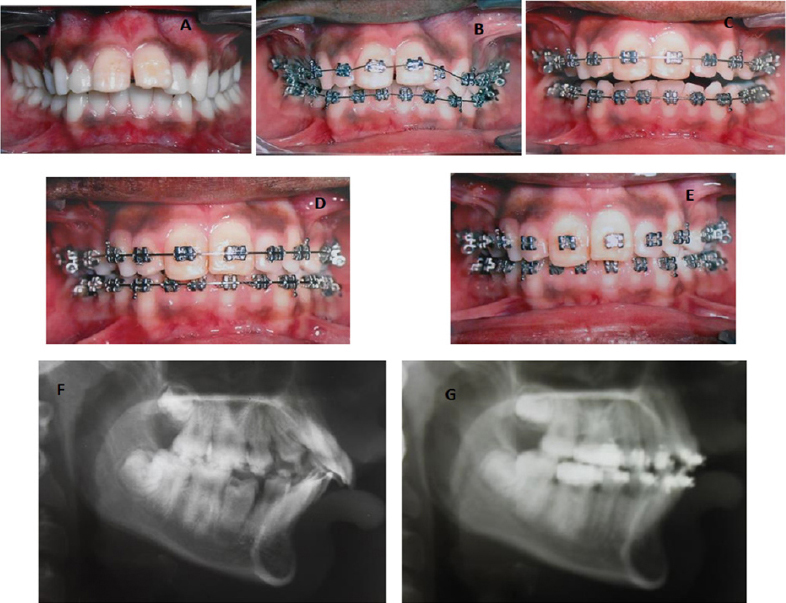
Many a time’s cases with thin alveolar bone will be presented to orthodontists (Figure 2), which pose challenge in deciding the treatment plan. Certain cases will be presented with the visibility of the root prominence (wash board appearance) because of the alveolar bone thinness and such cases if treated orthodontically would retain the root prominence after finishing the treatment (Figure 3). 17, 18
|
Figure 2: Case showing the thin alveolar bone in upper and lower anterior region and notice the retained root proximity to the cortical bone at the end stage of the treatment.
Click here to view |
|
Figure 3: Mandibular alveolar bone depicting the chances of Wash Board Appearance
Click here to view |
The long term prognosis of such finished cases reported in the literature is scanty.8, 19, 20 Nevertheless, the reported cases have shown the deleterious effects like root resorption and the gingival recession. As for the normal physiology goes the roots have to get resorbed in the long run because of the proximity to the alveolar bone and the friction between the two hard surfaces. But the question is does it really happen? If so, longitudinal studies should be conducted to check the prognosis of such cases. Bone remodeling is a boon in disguise for the orthodontist, because the bone remodels-the tooth moves. But the earlier studies have shown the limitation to this remodeling processes when the tooth touches certain anatomical limit.2-4 Thus, it is wise to go for the interdisciplinary approach like ortho-surgical approach or ortho-perio approach to treat such cases.
The results of the present study indicate that the alveolar bone thickness was not significantly different in different malocclusion groups except for the lower anterior alveolar bone width (LACW) which was significantly different for the class I and class II malocclusion groups. The lower posterior alveolar bone thickness in the class I malocclusion group was more in comparison to the class II malocclusion group. In class III malocclusion group the measurements like upper alveolar bone height and the lower alveolar bone height were increased in comparison to the other two malocclusion groups. Similar line of findings was reported in the previous study.8 Nevertheless contrasting results have also been reported, where they demonstrated significant differences between all the variables among the class I, class II and class III groups except for the anterior and posterior width of the lower anterior alveolus in the class III group.21, 22 The earlier study on the cephalometric norms for alveolar bone in the Saudi population, reported that the Saudi people had tendency towards thinner alveolus with increased proclination and protrusion of upper and lower incisors. When the results of the present class I group was compared with the Saudi people, it was found that the upper anterior and posterior alveolar width was more in the Saudi people.22
Upper posterior alveolar bone thickness was more in class II malocclusion group than the class I and class III group. This doesn’t come as surprise as maxilla will be prominent in the class II malocclusion cases. In the present study gender-wise difference was not taken into account, but in the previous study on the gender-wise difference for the alveolar bone thickness it was reported that there existed significant difference between males and females in all the malocclusion types.21, 22
Highly significant difference was noted for the height of the upper alveolar bone and the upper posterior alveolar bone thickness between the low and average mandibular divergence groups, where, the upper alveolar height was less and the upper posterior width was more in the low angle cases. Similar results were reported by Handelman, who reported lesser incidence of narrow alveolar bone in low angle cases in different types of malocclusion groups.8
However, for the low and high mandibular divergence groups, highly significant difference (<0.001) was found for the upper and lower alveolar bone height; the upper and lower posterior alveolar bone thickness. Contrastingly, for the average and high mandibular divergence group the highly significant difference was noted only for lower alveolar bone height. In the low mandibular divergence group, there was increase in the width alveolar bone at upper and lower posterior region, whereas in the high angle cases, increase in the height of the alveolar bone was noted in both the upper and lower region and the results were in accordance to the previous reports of the similar studies. Contrasting results are also been reported, where there existed no significant difference for the alveolar bone thickness for different mandibular divergence groups.23
Beckmann et al, in their study on the alveolar bone morphology of maxilla and mandible in the long face patients, reported that the mandibular midsagittal alveolar bone in the incisal region has limited anteroposterior dimensions and they advise to restraint antero-posterior movements of these teeth in long-faced patients.24 Same can be concluded in the present study as the lower anterior and posterior alveolar width was less in high angle cases.
The key to successful correction malocclusion with thin alveolar bone is following the interdisciplinary approach like going for the selective alveolar decortication (SAD) or periodontally accelerated osteogenic orthodontics (PAOO) technique or else orthognathic surgeries.17, 18, 25 The former two techniques don’t rely on the existing alveolar bone thickness.
CONCLUSION
The alveolar bone thickness varies according to the pattern of mandibular divergence in the present group of population. The type of malocclusion although influence the morphology of the alveolar bone, but to a lesser extent. The evidence provided can be enhanced by doing the similar kind of studies using advanced imaging technique and there existed a scope to check the difference between male and females for the anatomy of the alveolar bone.
