INTRODUCTION
The most spectacular technique in the innovation-oriented field of imaging is stereolithography. However there are still limitations such as the precision of details, which is dependent on technical limits (pixel size, slice thickness) and the artifacts of CT scanning, the representation of bone structures without contact with surrounding bone structures, and the cost of stereolithographic models.1 These become cost effective only if their application transcends from being merely illustrative to being undeniably valuable in the post operative planning of surgery and eventually the outcome of surgical procedure.
THE BASIC PROCESS2
-
Create a CAD model of the design
-
Convert the CAD model to STL format
-
Slice the STL file into thin cross sectional layers
-
Construct the model one layer atop another
-
Clean and finish the model
TECHNIQUE
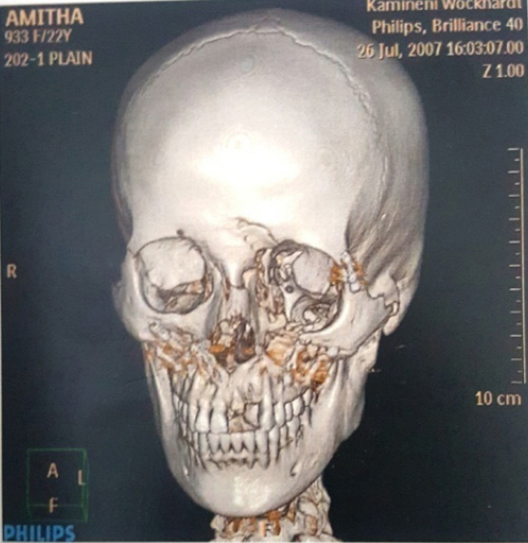
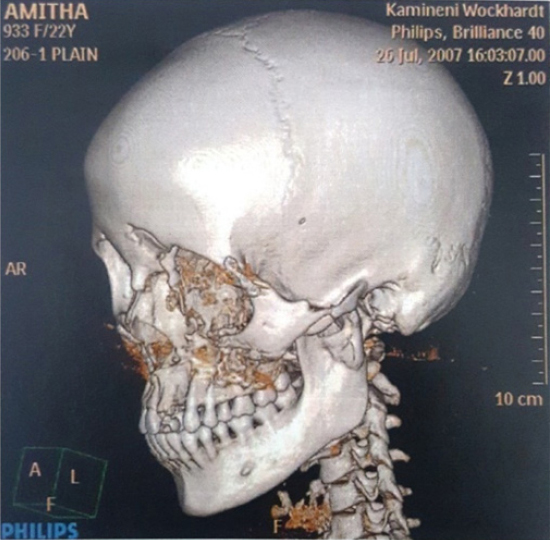
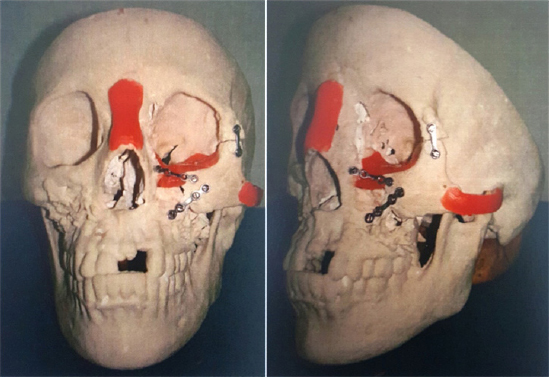
The preoperative CT images are obtained (Figure 1 & 2). A Stereolithography RP (Rapid Prototyping Technology) consists of a bath of photosensitive resin, a model building platform and an ultra violet (UV) laser for curing the resin. A mirror is used to guide the laser focus on the surface of the resin where the resin becomes cured when exposed to ultra violet radiation.3-6 The mirror is computer controlled its movements being guided to cure resin on a slice by slice basis. A model is initially designed with CAD software in a suitable file format (Commonly STL) and transferred to the stereolithographic machine for building. The CAD data file is converted in to individual slice of known dimensions. This slice data is the fed to the RP machine, which guides the exposure path of the UV laser on to the resin surface. The layers are cured sequentially and bond together to form a solid object beginning from the bottom of the model and building up. As becomes hardness. After layer of resin is exposed, the resin platform is lowered within the bath by a small known distance. A new layer of resin is wiped across the surface of the previous layer of using a wiper blade. And this second layer is subsequently exposed and cured. The process of curing and lowering platform in to the resin bath is repeated until the full model is complete. The self adhesive property of material causes the layers to bond to one another and eventually form a complete, robust, 3Dobject. The model is then removed from the bath and cured for a further period of time in a UV cabinet. The built part may contain layers which significantly over hang the layers below. If this is the case, then a network of support structures made of the same material is added beneath these overhanging layers at the design state, to add support during the curing process. These support structures analogous to a scaffold are removed by hands after the model is fully cured (Figure 3). This is a labor intensive and time consuming process. Generally, stereolithography is considered to provide the greatest accuracy and best surface finish of any RP technology. The model material is robust, slightly brittle and relatively light, although it is hygroscopic and may physically warp over time (a few months) is exposed to high humidity. The Osteotomy, Internal Fixation and Augmentation done on Bio-models was shown in Figure 4. The bio models provide a more realistic tool that is easier to handle than computer graphic images.7
|
Figure 1: 3D CT Image of skull showing frontal view
Click here to view |
|
Figure 2: 3D CT Image of skull showing lateral view
Click here to view |

|
Figure 3: Stereolithographic model showing residual deformity
Click here to view |
|
Figure 4: Bio-model showing the osteotomy, internal fixation and augmentation.
Click here to view |
The purpose of this paper was to assess whether stereolithography technology can assist in surgical treatment planning with regard to following parameters.
-
Preoperative planning and surgical simulation like:
-
Selection of implant i.e., size and shape.4
-
Evaluation of bone availability for placement of internal fixation.
-
Measurement of displacement after osteotomy, anticipation of size and form of bone graft.
-
-
Providing intra operative references during surgery as the model can be sterilized and can be brought into operating room.
-
Decreasing the intra operative time by allowing the surgeonsto rehearse incisions, measure grafts and fits surgical resections before they operate.5
SUMMARY AND CONCLUSION
Thus MRP (Medical Rapid Prototyping) modeling is undeniably valuable in the practice of oral and maxillofacial surgery. These models serve as indispensable tools for planning of complicatedmaxillofacial procedures such as correction of post traumatic defects, orthognathic surgeries, cleft alveolus and palate and transport distraction of the mandible. This technology is helpful in harvesting quantitative amount of bone graft from donor site, process of adapting the device and typing to fix it was longest and the most tedious part of surgery which also improved. After we started making models, the intra operative time was drastically reduced. The advantage of MRP technology in oral and maxillofacial surgical treatment can be summarized as follows:
-
Easy tolerated by the patient as it is noninvasive procedure.
-
Less expensive compared to models made by other MRP technologies, our method (3D) fabricates models that are relatively inexpensive, dimensionally accurate and reasonably strong and workable.
-
Quick to perform, less time consuming. The models can be fabricated in 1 to 2 days after CT scan is completed.
-
The post operative outcome of procedure is certainly better. Thus the models improve the prognosis.
-
Helps the surgeon to clearly visualize the osteotomy cuts for repositioning and alignment of bony fragments to their correct anatomical position.
