INTRODUCTION
Mucosal fenestration is a condition that can be described as breakdown of the overlying bone and alveolar mucosa leading to exposure of root apex in the oral environment. Mucosal fenestration can be caused due to malpositioning of teeth, prominent morphology of the root apex, thin alveolar cortex or severe periradicular inflammation with bone destruction. Mucosal fenestration has been most commonly found in the mandibular or maxillary anterior region, especially on the labial aspect because of tooth angulation placing root apices in a labial position.1,2 The various treatment options that have been reported for mucosal fenestrations include root canal treatment and root-end resection, full thickness mucogingival flap with primary or secondary healing, full thickness mucogingival flaps with guided tissue regeneration, bone grafting and pedicle flap surgeries.3,4
There has been a gradual shift in treatment protocol of teeth with open apex. The property of tissue to grow into the pulp space of a tooth with open apex is called revascularization.5 Disinfection with minimum instrumentation has been used resulting in high incidence of negative cultures.6 A double antibiotic paste of ciprofloxacin and metronidazole for 3-4 weeks adds to produce a pulp space free of bacteria and conducive for tissue regeneration. An intentional periapical instrumentation with a large hand file produces blood clot that acts as a scaffold or a source of growth factors promoting in growth of tissue from periapical area. Significant migration of undifferentiated mesenchymal cells occurs into the canal space by induction of periapical bleeding that has an important role in tissue regeneration.7
The present article reports a case series of 2 cases of apical fenestration in necrotic immature permanent teeth associated with apical periodontitis and mucosal breakdown where the soft and hard tissue defects were successfully treated by orthodontic correction of abnormal tooth root position that eventually led to closure of fenestration followed by regenerative endodontic management of immature root apex with apical periodontitis.
CASE REPORT
CASE 1:
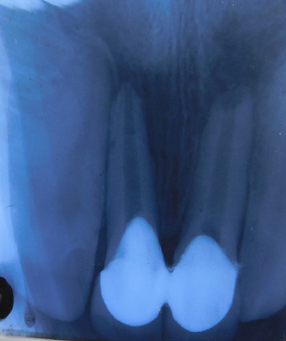
A 26 year-old female reported to department of conservative dentistry and endodontics, Banaras Hindu University with complaint of broken tooth in upper front region with ulceration in gums. There was a history of trauma 17 years back. On intraoral examination, root tip of tooth #11 was visible on its labial aspect and radiographic examination revealed an immature root-end in tooth #11 &21 with association of periapical radiolucency(fig 1&2). Thermal pulp testing was found to be negative in tooth #11&21. Periodontal probing depths were within normal limits without mobility of teeth. The diagnosis was necrotic immature tooth with asymptomatic apical periodontitis associated with labial mucosal fenestration. Orthodontic correction of abnormal root position followed by regenerative endodontic treatment of immature tooth was decided as the final course of treatment. An endodontic access opening was made using rubber dam isolation under local anesthesia that consisted of inferior alveolar nerve block and buccal infiltration by 2% lignocaine with 1:2,00,000 epinephrine. After determining the working length, the canals were instrumented, irrigated with 2.5% sodium hypochlorite and 17% EDTA and dried with paper points. A double antibiotic dressing was placed into the canal and a temporary restoration was given. Then, orthodontic correction of root tip was done presuming that root tip is too buccally in abnormal anatomical position. The patient was put on 020 slot pre adjusted edge wise MBT bracket system (American Orthodontics, Metal twin brackets). MBT bracket system was chosen as it has more build in anterior torque as compared to its immediate predecessor Roth’s prescription. Since the orthodontic treatment was an adjunctive treatment for the patient only upper arch was treated with the main aim to torque single tooth (Central Incisor). The initial alignment and levelling was done with 0.016-in niti wire, we gradually stepped up the wire from round 0.016-in to rectangular 0.019 x 0.025-in stainless steel wire. Stainless steel rectangular wires have a better control (two-point contact) on the tooth and are rigid. The wire was twisted 20 degrees in the region of central incisor before engaging the wire with ligature wires in the bracket slot.

|
Figure 1: Preoperative photograph showing root tip of tooth #11 on labial aspect.
Click here to view |

|
Figure 2: Preoperative IOPA radiograph shows an immature root-end in tooth #11 & 21 along with periapical radiolucency
Click here to view |
After orthodontic correction of tooth root, it was noticed that complete healing of mucosal fenestration defect had occurred and the patient was completely asymptomatic(fig3). The root canal was then irrigated with 2.5% sodium hypochlorite and 17% EDTA and dried with paper points. A double antibiotic dressing was placed into the canal and a temporary restoration was given. After 4 weeks the teeth were reopened, irrigated with 2% chlorhexidine and dried with paper points and then PRF made from patients own blood (by centrifuging 5 ml of venous blood at 2700 rpm for 12 minutes) was introduced into the canals and carried to the apical part of root canals using endodontic pluggers and access cavities were sealed with glass ionomer cement. Recall visits were scheduled at 6 months and 12 months interval. At 6 months recall, patient was asymptomatic showing partial healing of periapical radiolucency. At 12 months recall, patient was asymptomatic. Hence porcelain fused metal crown was given as permanent restoration(fig4).

|
Figure 3: Picture showing complete healing of mucosal fenestration defect after orthodontic treatment.
Click here to view |
|
Figure 4: Radiograph showing complete healing after 12 months
Click here to view |
CASE 2:
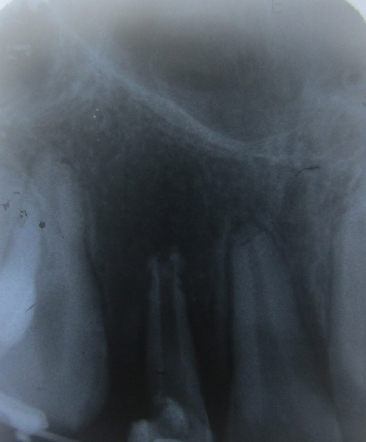
A 20-year-old male reported with a complaint of discolored upper front teeth. Patient gave a history of fall 10 years ago. On examination, upper right lateral incisor was discolored and also non-vital on pulp testing. Clinical examination showed labial inclination of root tip of maxillary right lateral incisor leading to mucosal fenestration(fig5). Radiographic examination of tooth #12 revealed an immature apex with associated periapical radiolucency(fig6). Periodontal probing depths was within normal limits and there was no mobility of tooth. Orthodontic correction of root position followed by regenerative endodontic therapy of immature tooth was proposed as treatment. After access opening under rubber dam isolation, local anaesthesia (2% lignocaine with 1:2,00,000 epinephrine) as inferior alveolar nerve block and buccal infiltration was given. After determining the working length, the canals were instrumented, irrigated with 2.5% sodium hypochlorite and 17% EDTA 10ml and dried with paper points. A double antibiotic dressing was placed into the canal and a temporary restoration was given. Orthodontic treatment was then implemented in the same way as case I for correction of tooth position. After orthodontic torquing of tooth root, mucosal defect was clinically found to heal completely(fig7). Then, the tooth was reopened, irrigated with 2% chlorhexidine and dried with paper points and then bleeding was induced into the canal using a no.50 k file. Collagen granules were soaked into the normal saline solution and placed into the canal with the help of endodontic plugger up to the CEJ and access cavity was sealed with glass ionomer cement. The patient was asymptomatic with continuation of periapical healing at 12 month(fig8). So tooth was permanently restored with porcelain fused metal crown.

|
Figure 5: Preoperative photograph showing labial inclination of root tip of maxillary right lateral incisor leading to mucosal fenestration.
Click here to view |

|
Figure 6: Preoperative radiograph reveal an immature apex along with periapical radiolucency with tooth #12
Click here to view |

|
Figure 7: Mucosal defect was clinically found to heal completely after orthodontic treatment
Click here to view |
|
Figure 8: Radiograph showing complete periapical healing after 12 months.
Click here to view |
DISCUSSION
Fenestration of the root apex is a relatively uncommon complication of pulpal-periradicular disease. The probable aetiological factors in the cases reported were extreme buccal inclination of root tips with very thin or nonexistent buccal cortical plate, combined with chronic periradicular inflammation. Mucosal breakdown and exposure of the root tip to the oral cavity leaves the root-tip vulnerable to plaque accumulation and calculus formation. These events make spontaneous soft-tissue coverage of the exposed root-tip improbable. If the bony or mucosal defect is small, a better-coloured local pedicle soft tissue may be sufficient to cover the defect, and primary closure may be indicated to prevent the aesthetic risk. On the other hand, large bony or mucosal defects will have only minimal buccal bone plate support and insufficient blood supply for tissue repair or regeneration. Successful management of periapical mucosal fenestration requires correct diagnosis and treatment procedures including adequate debridement of the root canal and reconstruction of bony and mucosal defects.8,9 The present case series is amongst the first few where orthodontic intervention combined with endodontic approach led to mucosal fenestration coverage. The possible cause behind healing of mucosal defect may be assumed to be the etiology of fenestration in present cases that was probably labial inclination of root tip and chronic periradicular inflammation. Correction of mucosal defect needs to create an environment for successful periapical healing, which in the present case was obtained by sterilization of the canal by effective irrigation and use of double antibiotic dressing in the canal that has proved to create almost complete aseptic condition. Orthodontic closure of defect has advantage over earlier used periodontal surgical methods that apart from being non surgical procedure it restores the tooth root to its normal position that is otherwise not considered in surgical approaches and that’s how furnishes space for new bone formation in a natural way by providing aseptic condition conducive to new bone formation.
Torque is a force system. It is produced by torsion in an arch wire that creates a couple when interacted with a bracket slot, which is the result of twist in the wire compared to the bracket slot. Torque is not in the wire or not the angle of the bracket slot which are the common myth.
Torque applied to a tooth created by torsion in the arch wire against the bracket slot spins the tooth around its centre of resistance. In orthodontics mechanics, 3rd order twist in the arch wire produces a torque.
Clinically there are two types of torque either lingual root torque or buccal root torque if we are talking in reference to the root or same can be applied to crown i.e. lingual/palatal crown torque or buccal crown torque. The force system can be applied either on a single tooth, multiple tooth by differential bending / twisting the wire or progressive torque.
Torqueing in the upper anterior dentition is of utmost importance as it decides for the micro aesthetics. The amount of torque needed can be assessed by lateral cephalogram or computer tomography methods. The orthodontic brackets have in built tip and torque therefore in order to express it to fullest one has to engage a rectangular wire of 0.019 x 0.025-in stainless steel or 0.021 x 0.025-in stainless steel dimension, which can fill the slot completely twisting the wire to express torque. There can be occasions when a clinical case may require extra torque to bring the position of root to its normal position for achieving stable results.
The cases presented here, have their roots buccally displaced due to periapical pathology leading to development of fenestration. A fenestration10 is said to be an isolated alveolar bone defect leading to exposure of root surface without involving the marginal alveolar bone. Whereas it is considered as dehiscence when there is the absence of at least 4 mm of cortical bone apical to the margin of interproximal bone. The development of fenestration and dehiscence may require a surgical intervention in term of flap surgeries / bone grafting procedures.
There can be different etiological factors leading to development of fenestration. If a tooth is buccally placed in the arch, the bone may get denuded exposing the root at about 1-1.5 mm from CEJ11. If the fenestration is present at apical level in a tooth having peri radicular pathology, the protruding root apex is re-contoured, the root is cleaned, and root end is filled to allow alveolar bone regeneration which seems to be a common practise. A closer look at the position of the root will show that the root apex is still in abnormal position i.e. they are more buccally placed. A more conservative and novel treatment option can be, torqueing the root to its normal position and allowing the mucosa and alveolar bone to heal. A thorough root cleaning would be required prior to torqueing the root.
The excellent elasticity and strength of PRF membrane is attributed to prolonged and natural polymerization of the collected blood, accompanied by physiologic concentrations of thrombin. Role of PRF in bone regeneration while sinus floor elevation was reported by Choukroun et al. who displayed that histologic maturation of the PRF group after 4 months healing time, was similar to that of the control group that was for a period of 8 months. According to Dohan et al.12 PRF in Choukroun’s experiment simultaneously stimulated proliferation of oral BMSC and sort of differentiation in a dose-dependent manner, that was characterized by a strong alkaline phosphatase activity, with the formation of nodules that were mineralized. According to Su et al. since maximum release of growth factors from PRF occurs in first 60 minutes, it should be used on the surgical sites preferably before this period has elapsed.13 The present study followed this protocol and prepared PRF was used within this period. PRF membrane because of its smooth surface might possibly promote cell proliferation better than other scaffolds which have rough surfaces, as smooth surfaces are known to promote proliferation better than rough surfaces.
The study of Yamauchi et al on animals that included placement of cross linked collagen scaffold in combination with blood clot resulted in increased deposition of mineralized tissue on the root canal walls.14 They concluded that increase in vital support structure resulted due to the thickening of root structure with cementum like tissue.
The present case series suggests that orthodontic closure of bony defect combined with regenerative procedure with PRF or collagen as scaffold for immature apex has better predictability compared to lateral pedicle flap, Guided Tissue Regeneration (GTR) and apicoectomy combined with endodontic, as it provides more space for bone formation in the defect area and being completely non invasive approach in contrast. The possibility of successful tissue repair appears not to be precluded by restraints of failed conventional treatment, narrow canal & foramen size.
CONCLUSION
Mucosal fenestrations and dehiscence although are rare conditions but pose a difficult situation for the clinician whenever present,. Larger defects may raise the challenge compromising the prognosis. Various non surgical and surgical procedures have been documented for its treatment. The present case series describes a new approach where a mucosal fenestration developed in the upper left central incisor was successfully treated with combination of orthodontic and regenerative endodontic therapy, bestowing the procedure as a viable treatment option in such cases.
