INTRODUCTION
Ameloblastic fibromas are a rare variety of benign odontogenic tumors composed of proliferating odontogenic epithelium embedded in a cellular ectomesenchymal tissue resembling dental papilla.1 It was first described by Kruse in 1891 and later classified as a separate entity by Thoma and Goldman in 1946.2, 3 It can appear in either the maxilla or mandible, with the posterior region of the mandible as its most common anatomic site. Diagnosis is generally made through routine radiographic examinations performed to look for an impacted tooth as a cause of the swelling.4 Conservative excision seems to be the treatment of choice for ameloblastic fibroma. A modified block resection, rather than a curettage or simple excision, has been suggested.5
CASE REPORT
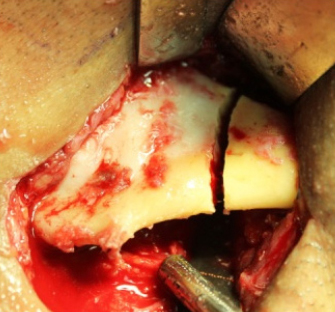
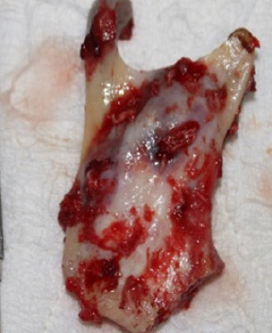
A 45 year old male patient reported to the department of oral & maxillofacial surgery, with the chief complaint of a swelling in the right lower jaw since 6 months. The swelling was insidious in onset and gradually increased to the present size. Extraoral examination revealed adiffuse swelling measuring 2 x 2 cm on the right side of the mandible, extending anterio-posteriorly 2 cm posterior to the right corner of the mouth to the angle of the mandible (Figure 1). Swelling was not associated with any symptoms like pain. Intra oral examination revealedswelling extending from distal aspect of second molar to the anterior border of ramus of the mandible causing vestibular obliteration which is non tender and hard in consistency. On lingual aspect, swelling was mildly perceptible and the overlying mucosa was intact and normal in color. Orthopantomograph revealed a well defined unilocular radiolucent lesion with sclerotic radiopaque marginsextending from 37, involving impacted third molar, ramus up to coronoid process and subcondylar region of right side of mandible (Figure 2). The CT findings revealed expansion of buccal and lingual cortical plates andperforation of the lateral aspect of ramus of the mandible (Figure 3). Based on the clinical and radiological examinations, a provisional diagnosis of ameloblastoma was made. An incisional biopsy was done providing a diagnosis of ameloblastic fibroma. Considering the aggressive nature of ameloblastic fibroma, resection of the lesion followed by reconstruction with iliac crest graftwas planned. Submandibular incision was given 2cm below inferior border of right side of mandible and layer wise dissection done. Facial artery and vein were identified and ligated. The lesion was exposed and the segmental resection of the mandiblewas carried out using a gigly saw with a safety margin of 1 cm extending anteroposteriorly from distal aspect of right first molar region to condyle along with the coronoid process (Figure 4 and 5).

|
Figure 1: Preoperative clinical photograph showing swelling in the right angle region
Click here to view |

|
Figure 2: Preoperative radiograph showing radiolucency involving the right ramus and angle of the mandible
Click here to view |

|
Figure 3: Preoperative 3D CT showing cortical expansion due to ameloblastoma involving the right ramus
Click here to view |
|
Figure 4: Intraoperative photograph showing the osteotomy cut for the resection of the ameloblastoma
Click here to view |
|
Figure 5: Photograph showing the sected ramus with the ameloblastoma lesion
Click here to view |
For harvesting the iliac graft, a sub-crestal window technique was performed by making skin incision over the anterior iliac crest. Muscles were stripped sub-periosteally from the ilium, and the cortico-cancellous block of length 4 cm was harvested by using osteotomes (Figure 6). Following the removal of the bone graft, hemostasis was achieved and a drain was placed into the site followed by closure of the periosteal layer. The muscle layers and subcutaneous tissue were closed with 3-0vicryl. The skin was closed with 3-0 prolene (interrupted sutures).

|
Figure 6: Intraoperative photograph the harvesting of iliac graft
Click here to view |
The reconstruction plate was contoured and the condylar segment from the resected specimen was sectioned and fixed as a free graft. Stabilization of the harvested iliac crest graft was done using 2.5 x 10 mm titanium screws (Figure 7 and 8). Layer wise closure was done with 3-0 vicryl and 5-0 prolene extra orally). Excisional biopsy confirmed the diagnosis as ameloblastic fibroma. The patient has been followed up periodically till 3 years. The outcome has been aesthetically satisfactory and there have been no signs of recurrence.

|
Figure 7: Intraoperative photograph showing reconstruction of the resected segment with iliac graft and reconstruction plate
Click here to view |

|
Figure 8: Postoperative radiograph showing reconstruction of the resected segment with iliac graft and resected condylar segment secured with reconstruction plate
Click here to view |
DISCUSSION
Ameloblastic fibroma is a true histologicbiphasic tumor because epithelial and mesenchymal components are part of the neoplastic process. According to Reichart and Philipsen, male to female ratio was 1.4:1. Mean age of occurrence is 14.8 years with a range of 0.5 to 62 years. It is a slow growing tumor which is commonly located in the mandibular posterior area and is often associated with an impacted tooth. Philipsen et al. proposed that the innocuous behavior of the lesion does not justify aggressive initial treatment but rather meticulous surgical enucleation with close clinical follow-up.4 Muller et al reported that since 1960, 44% cases of ameloblastic fibrosarcoma (19/43) had arisen from ameloblastic fibroma.6 A recurrence rate of 43.5% and 18% was reported by Trodahl and Zallen, respectively. Gundlach was of the opinion that simpleenucleation would not be sufficient for ameloblastic fibroma.7 An aggressive surgical treatment is, therefore, suggested by some authors because of the possibility of malignant transformation of an ameloblastic fibroma to an ameloblastic fibrosarcoma. A modified block resection of the mandible with the placement of an immediate autologous bone graft is treatment option for an extensive tumor and/or multiple recurrences. Complete excision of the tumor with long-term clinical and radiographic follow up is highly recommended.8