INTRODUCTION
Sturge-Weber syndrome (SWS), or encephalotrigeminal angiomatosis, is a rare, congenital neurocutaneous syndrome characterized by unilateral facial cutaneous vascular malformation (nevus flammeus or port-wine stain [PWS]) in association with ipsilateral leptomeningeal angiomatosis.[1] It was first described by Sturge in 1879 in a 6-year-old girl with facial nevus, and later, cerebral involvement was demonstrated by Kalischer in 1897[2] It is often associated with seizures and other neurologic complications, including mental retardation, contralateral hemiparesis, and glaucoma.[3] Prevalence of the disease among the neurocutaneous syndromes, especially with vascular predominance, is 1/50,000 live births and no racial bias.[4] Both the genders are affected equally. Intraorally, angiomatosis can involve lips causing macrocheilia, resulting in hemihypertrophy of the buccal mucosa, palate, and the floor of the mouth. Vascular hyperplasia is most commonly seen involving gingival.[4] Failure of its regression results in residual vascular tissue which forms angiomas of leptomeninges, face and ipsilateral eye. These blood vessels show abnormal blood flow pattern as vasomotor phenomenon, venous occlusion, thrombosis and “vascular steal phenomenon” resulting in ischaemia, gliosis, atrophy and calcification of underlying cortical tissue. Although the leptomeningeal angioma in SWS is typically a static lesion, it has been demonstrated by some to be of progressive nature.[5]
CASE REPORT
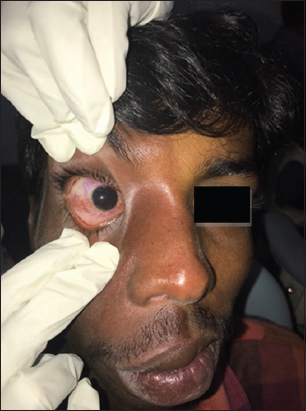
A 23-year-old male patient was referred to the Department of Oral Medicine and Radiology with a chief complaint of swollen gums. On medical history, he had no history of seizures. The patient was observed to have a normal intelligence, a moderate build, and normal temperature, pulse, respiration, and blood pressure. On extraoral examination, a hemihypertrophy was observed on the right side of the face extending from hairline till lower border of mandible along the division of the trigeminal nerve with PWS which was present since birth [Figure 1]. Mouth and nasal septum were deviated toward the right side of the face. Glaucoma was seen involving the eye [Figure 2]. Intraoral examination revealed soft, non-tender vascular hyperplasia involving gingiva in right upper quadrant of the oral cavity, and a solitary well-defined ulcer of size 0.8 × 1 cm is seen on swelling in gingiva due to trauma which is tender on palpation [Figure 3]. Red pigmentation was observed over the upper and lower labial mucosa [Figure 4], buccal mucosa, palate, and ventral surface of the tongue on the right side [Figure 5]. Hypertrophy of the upper and lower lip is present [Figure 6]. On diascopy test, blanching was seen in the upper and lower lip and maxillary gingival on the right side [Figure 7].

|
Figure 1: Clinical picture showing port-wine stain on the right side of face
Click here to view |
|
Figure 2: Clinical picture showing glaucoma involving the right eye
Click here to view |

|
Figure 3: Intraoral examination showing vascular hyperplasia involving gingiva in right upper quadrant
Click here to view |

|
Figure 4: (a and b) Intraoral examination showing red pigmentation in the upper and lower labial mucosa
Click here to view |

|
Figure 5: (a-c) Intraoral examination showing red pigmentation in the buccal mucosa, hard palate, and ventral surface of tongue on the right side
Click here to view |

|
Figure 6: Hypertrophy of the upper and lower lip
Click here to view |

|
Figure 7: (a-c) Positive diascopy test
Click here to view |
Differential diagnosis of Klippel–Trenaunay–Weber syndrome in which PWSs are seen in extremities and face, hemihypertrophy of soft and bony tissues, and Beckwith–Wiedemann syndrome along with facial PWS, macroglossia, omphalocele, and visceral hyperplasia, other lesion syndrome, and coats disease were considered.
Investigations that were carried out in the present case included an orthopantomograph (OPG), lateral skull view, and complete hemogram. The OPG revealed hemifacial hypertrophy in the right side of face [Figure 8]. The complete hemogram showed normal hemoglobin levels with no other abnormality in the total or differential white blood cell counts. Bleeding and clotting time were within normal limits. Lateral skull view showed no abnormalities such as calcification, atrophy with dilatation of ventricle, and enlargement of sinuses. The presence of glaucoma was confirmed by ophthalmologist. Based on the clinical findings and radiological findings, diagnosis of SWS was given.

|
Figure 8: Orthopantomogram showing hemifacial hypertrophy is seen on right side
Click here to view |
DISCUSSION
SWS is a typical neurocutaneous syndrome which is uncommon, non-familial, congenital condition of unknown etiology. It is often associated with capillary or cavernous hemangiomas affecting primarily but not limited to cutaneous distributions of the trigeminal nerve and rarely venous malformations involving leptomeninges that lead to progressive destruction of the adjunct cerebral cortex.[6] Most commonly involves one or more unit of trigeminal nerve unilaterally.[7]
It is believed that SWS results from a developmental defect in the 1st month of gestation, represented by the persistence of a vascular plexus which develops in the 6th week of intrauterine life, but normally undergoes regression during the 9th week around the cephalic portion of the neural tube. The association between cerebral angiomatosis and facial nevus, characteristic of the syndrome, is attributed to the development of the skin of the face from the ectoderm that covers this vascular plexus.[3]
When both cranial nervous system and facial angiomas are present, SWS is referred to as complete and incomplete when only one area is affected without the other. It is classified into three types based on roach scale: Type I - both facial and Las - may have glaucoma, Type II - facial angioma alone (no central nervous system [CNS] involvement) - may have glaucoma, and Type III - isolated LAs - usually no glaucoma.[8]
In the present case, there was ocular involvement with glaucoma, and facial angioma was unilateral present since birth with vascular hyperplasia involving gingival in the affected quadrant (right maxillary) without any CNS manifestations leads to a diagnosis of SWS Type II according to Roach classification.
According to Inan, the port-wine nevus is localized on the face, especially over the right side, and is detected in 87–90% of the cases. The lesion extension over the middle line is observed in 50% of the patients and bilateral involvement can be detected in about 33% of the cases.[9]
The ipsilateral leptomeningeal angiomatosis also represents one of the main signs of the syndrome, may present with a progressive nature, and commonly leads to cerebral calcifications, epileptic convulsive crises, contralateral hypertrophy, hemiparesis (30%), and mental retardation (50%).[4] Facial lesions are the other characteristic feature of this syndrome and include rosy-purple nevus flammeus lesions that are sharply demarcated and usually flat; these occur on the ipsilateral side of the face in 90% of the patients, which may extend onto the neck, chest, and back. The facial features also may include hemihypertrophy of the involved side of the face. Ocular involvement may present in the form of choroidal angioma, glaucoma, hemianopsia, or buphthalmos (enlargement of the coating of the eye). Oral manifestations are present in approximately 38% of the cases, and they may involve hemangiomatous lesion in the lip, oral mucosa, gum, tongue, and palatine region.[10]
Neuroimaging studies include skull radiograph, angiography, CT scan, magnetic resonance imaging (MRI), MRI with gadolinium, and functional imaging with single-photon emission computed tomography (SPECT) or positron-emission tomography (PET). CT scan and skull radiograph may show the characteristic gyriform intracranial “tramline,” or “tram-track” or “trolley-track,” calcifications located in the cortex underlying the leptomeningeal vascular malformations, cerebral atrophy, and enlargement of the medullary and subependymal veins and the choroid plexus.[11] Calcifications appear as areas of decreased signal intensity on spin density and T2-weighted MR images.[12] Cerebrospinal fluid shows elevated levels of proteins. Angiography shows lack of superficial cortical veins, non-filling dural sinuses, and abnormal torturous vessels. SPECT shows early hyperperfusion and late hypoperfusion. PET shows hypometabolism. Reduced background activity, polymorphic delta activity, and epileptiform features are seen in electroencephalogram.[13]
The primary aim of pharmacologic treatment is to minimize or optimally eliminate seizure activity. Anticonvulsants are most commonly used such as oxcarbazepine, levetiracetam, and topiramate. If seizures persist surgical procedures such as functional hemispherectomy, anatomic hemispherectomy, and hemispherectomy can be done. Opthalmologic symptom most commonly seen is glaucoma and can be effectively treated by topical medication latanoprost. Common surgical therapies include trabeculectomy, trabeculotomy, and goniotomy in infants and children, as well as valve drainage implants, non-penetrating sclerectomy, procedures in adults.[14]
Skin manifestations such as port-wine birthmark can be treated by lasers. Flashlamp-pumped PDL is the current method for lightening port-wine birthmarks, which targets the port-wine vasculature without affecting the surrounding epidermis or dermis.[15]
The dental rehabilitation in cognitive/psychological function impairment patients is a complex process, requiring conservative management, and may demand the use of behavior management techniques due to mental retardation specialized education services, behavioral psychology intervention, and stimulant use in patients with cognitive deficits and attention problems have shown to be benefited.[16] Conscious sedation can be used when required. Whenever oral surgery is planned in SWS patients, particular care must be paid to achieve hemostasis during and after the surgical procedure by splints, injection of anesthetic solutions with vasoconstrictors. In spite of strict oral hygiene measures, angiomatous gingival enlargement poses a threat to gingival health and may at some point require gingivectomy. Nd: YAG and CO2 lasers can be used for gingivectomies in SWS patients with good safety.[3]