INTRODUCTION
Endodontic therapy primarily aims at the elimination of microbes and tissue debris from the infected root canals by thorough biomechanical preparation followed by three-dimensional obturation with a hermetic seal to prevent further reinfection. Missing additional roots/canals are one of the frequent causes of failure of non-surgical root canal therapy. Mandibular first molars are considered to be most frequently involved tooth in endodontic practice as they erupt early and are known to display several anatomic variations. Hence, an in-depth knowledge of the aberrant morphology should be obtained by the clinician for the successful outcome of endodontic therapy.[1,2]
The mandibular first molars are usually two rooted with two mesial and one distal canal.[1,2] In majority of cases, mesial root has two canals, ending in two distinct apical foramen or sometimes they merge at the root top to end in one foramen. Distal root usually presents an oval kidney-shaped single canal, although two canals may be present with narrow and round orifices.[3] However, Fabra-Campus and Bond reported the presence of three mesial canals while Stroner reported three distal canals.[4-7] Like the canals, number of roots may also vary. In 1844, Carabelli first mentioned an extra root on the distolingual position of permanent mandibular first molar and termed radix entomolaris (RE).[8] If the extra root is on buccal aspect, it is referred as radix paramolaris (RP).[9] The reported prevalence of RE significantly differs with races ranging from 0 to 33.1%.[10] In Indian population, occurrence of RE and RP is <5% and not routinely observed. Hence, knowledge of the extra roots and canals and radiographs taken at different angulations is essential for delivering a successful endodontic treatment.
CASE REPORTS
Case 1
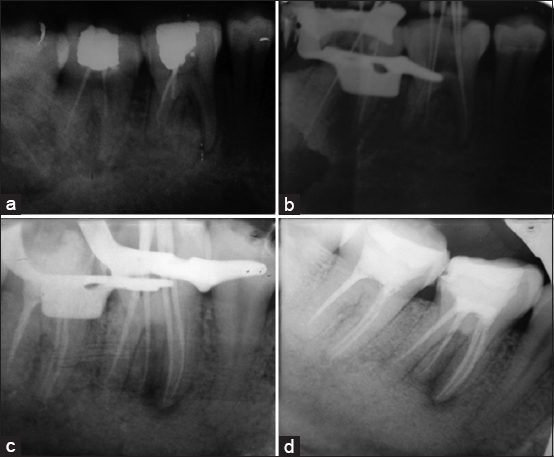
A 25-year-old female patient reported to the department of conservative dentistry and endodontics with pain on the right lower back region which was intermittent for last 2 weeks. The patient reported a history of endodontic therapy done on 46 and 47, 4 months back. The patient’s medical history was non-significant. Clinical examination revealed amalgam restoration on 46 and 47, and both were mildly tender on percussion. Radiograph [Figure 1a] revealed incomplete obturation on both 46 and 47 and an extra root on 46. A diagnosis of previously treated tooth with symptomatic apical periodontitis on 46 and 47 was made. Non-surgical retreatment of 46 and 47 was planned.
|
Figure 1: (a) Pre-operative radiograph reveals incomplete obturation in 46 and 47 and an extra root in 46, (b) radiograph showing working length determination using electronic apex locator Root Zx, (c) radiograph showing master cone suitability of gutta-percha to canals, (d) post-operative radiograph showing endodontic restoration in 46 and 47 with amalgam
Click here to view |
The patient was given local anesthesia of 2% lignocaine with 1:80,000 adrenaline. Both 46 and 47 were isolated with rubber dam (GDC India). The amalgam restoration of 46 was removed and access gained into the pulp chamber. The two mesial canals were not obturated and gutta-percha was found on distal canal. An extra canal with GP on it was found buccally between the mesial canals and distal canal. Access opening was little bit modified to become roughly trapezoidal so that there would be an easy access to extra canal of RP. GP was removed from both the canals. The extra canal was approached from the lingual aspect of the crown and patency of the canal was made with 15 number K-file (Dentsply Maillefer Company, USA). Access opening was done on 47 also. Two mesial and one distal canal were located and GP was removed. Working length was determined using electronic apex locator Root ZX (J. Morita MFG. Corporation, Kyoto, Japan) which was confirmed using periapical radiograph [Figure 1b]. The canals were cleaned and prepared using hand K-files (Dentsply Maillefer Company, USA) on step-back technique. 2.5% sodium hypochlorite was used an irrigant. The intracanal medicament of calcium hydroxide (Prime Dental Products, Thane) was given for 1 week. After 1 week, teeth were asymptomatic. Root canals were reaccessed; intracanal medicament was removed and dried using paper points. Master cone radiograph [Figure 1c] was taken to confirm the suitability of gutta-percha to canals. The canals were obturated with selected master gutta-percha cones, accessory cones, and zinc oxide-eugenol sealer using lateral condensation technique. A temporary restoration was given with Cavitemp. After 1 week, post-endodontic restoration was done on 46 and 47 with amalgam [Figure 1d].
Case 2
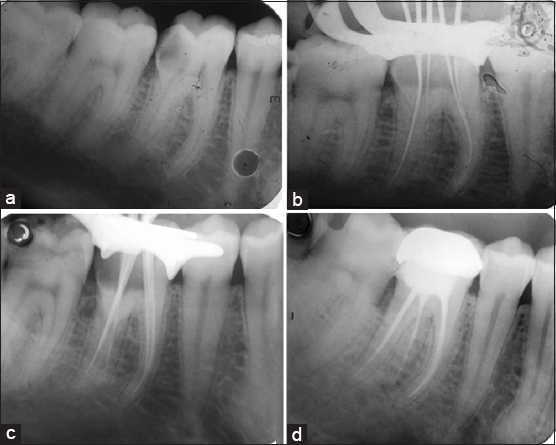
A 26-year-old male reported to the department of conservative dentistry and endodontics with pain in relation to the lower right back region for last 3 days. The patient medical history was not significant. Clinical examination revealed the presence of deep distoocclusal caries on right mandibular first molar. Thermal test showed positive and prolonged response. Periapical radiograph [Figure 2a] revealed radiolucency overlapping the pulp chamber from distoocclusal aspect. It also suggests an extra root toward the distal root complex. Diagnosis of symptomatic irreversible pulpitis was confirmed and non-surgical endodontic therapy was planned.
|
Figure 2: (a) Pre-operative radiograph showing periapical radiolucency overlapping the pulp chamber from distoocclusal aspect. It also suggests an extra root toward the distal root complex, (b) radiograph showing working length determination using electronic apex locator Root ZX, (c) radiograph showing master cone suitability of gutta-percha to canals, (d) post-operative radiograph showing endodontic restoration in 46 with amalgam
Click here to view |
Local anesthetic of 2% lignocaine with 1:80,000 adrenaline is administrated and conventional endodontic access was made under rubber dam (GDC India) isolation. On deroofing of pulp chamber, we found two mesial canals and two distal canals. On modifying the access cavity toward the distolingual side, an extra canal was found suggestive of RE. The patency of canals was made with 10 number K-file (Dentsply Maillefer Company, USA). Working length was determined using electronic apex locator Root ZX (J. Morita MFG. Corporation, Kyoto, Japan) and confirmed radiographically [Figure 2b]. Biochemical preparation was done with Rotary Hyflex CM file system using crown-down technique. 2.5% sodium hypochlorite was used as irrigant and calcium hydroxide as interappointment medicament. The patient was recalled after 1 week and obturation was done with gutta-percha and zinc oxide-eugenol sealer using lateral condensation technique [Figure 2c and d]. Cavitemp was given as temporary restoration. 1 week after, permanent restoration was done with silver amalgam.
DISCUSSION
The etiology of RE is still unclear. The prevalence of RE ranges from 0 to 33.1% differing significantly between races. The prevalence in high among mongoloid group with >30% and considered to be eumorphic root morphology.[11-13] In African, Eurasian, Caucasian, and Indian population, it is considered as dysmorphic root morphology with a low prevalence of <5%.[12-13] In dysmorphic roots, it occurs due to external factors during odontogenesis or attribution to atavic gene or polygenic system.[11,13] The more pronounced phenotypic manifestation of a particular gene under the influence of racial and genetic factors may be the reason in eumorphic roots.[14,15] Slight male predilection is reported in some studies (16) and bilateral occurrence ranges from 37.14 to 67%.[16-18]
Bolk reported the occurrence of RP but occurs less frequently than RE.[19] According to Visser, the prevalence of RP was 0% for mandibular first molars, 0.5% for second molars, and 2% for third molars.[20]
Classification
Carlsen and Alexandersen classified RE into four different types based on the location of its cervical part[9]:
-
Type A: The RE is located lingually to the distal root complex which has two cone-shaped macrostructures.
-
Type B: The RE is located lingually to the distal root complex which has one cone-shaped macrostructures.
-
Type C: The RE is located lingually to the mesial root complex.
-
Type AC: The RE is located lingually between the mesial a distal root complexes.
De Moor et al. classified RE based on the curvature of the root or root canal [21]:
-
Type 1: A straight root or root canal.
-
Type 2: A curved coronal third which becomes straighter in the middle and apical third.
-
Type 3: An initial curve in the coronal third with a second buccally oriented curve which begins in the middle or apical third.
Song et al. further added two more newly defined variants of RE[22]
-
Small type: Length shorter than half of the length of the distobuccal root.
-
Conical type: Smaller than the small type and having no root canal within it.
Classification of RP
Carlsen and Alexandersen (1990) classified RP into two different types [9]:
-
Type A: Cervical part is located on the mesial root complex.
-
Type B: Cervical part is located centrally, between the mesial and distal root complexes.
Clinical implications
Since RE and RP are rare in Indian population, missing of the extra root can happen as the first case reported here. Hence, an accurate diagnosis of these supernumerary roots can avoid complications is the endodontic procedures. A thorough inspection of the pre-operative radiograph and interpretation of particular marks such as unclear view or outline of distal or mesial root contour of root canal can suggest the presence of radix cases. In such cases, additional radiograph taken from different horizontal projections (20°from mesial/distal) reveal information on additional root.[20,23] In cases of RE and RP, the access opening has to be modified to more rectangular or trapezoidal form. The use of magnifying loupes or dental microscope will be helpful. The dentinal map on the purple floor usually helps in getting precise location of these extra roots. Most of the times RE and RP have serve root inclination or curvature, particularly in apical third and can lead to procedural errors such as ledges, transportation, and instrument separation. Hence, initial canal exploration with small files, use of NiTi files, and creating a glide path before biomechanical preparation tooth has to be considered.
In other specialties, considerations include RE and RP may pose difficulty during extraction and tooth movement may be difficult in orthodontic procedures.
CONCLUSION
The clinicians should always be aware of unusual root morphologies such as extra canals and roots while treating mandibular molars. An initial diagnosis of RE and RP is of utmost importance to facilitate successful endodontic therapy. Radiographs taken at different horizontal angles may help in the diagnosis. A careful clinical approach is needed in cases of RE and RP to give a successful result without any procedural complications.
