INTRODUCTION
Nickel allergy is by far the most common contact allergy in the industrial world, with a prevalence of up to 30%, depending on age, sex, and ethnicity.1, 2 Possible sources for nickel sensitization include jewellery, clothing fasteners, mobile phones, and, in particular, (ear) piercings.
Nickel allergy a concern for the orthodontist because it is present in a vast array of materials frequently used in orthodontics. Nickel is the most common component of the super-elastic nickeltitanium (Ni-Ti) archwires used during the initial levelling and aligning phase of orthodontic treatment with a concentration of 47-50%.3 It is also a component in stainless steel (present in both archwires and brackets), representing approximately 8% of the alloy. Extraoral orthodontic appliances such as the outer bows of headgears contain nickel and may also elicit a response on the skin.4
Biology and Immune Response of Nickel Allergy
The response by the immune system to nickel is usually a Type IV cell mediated delayed hypersensitivity also called an allergic contact dermatitis. It is mediated by T-cells and monocytes/ macrophages rather than antibodies and consists of two phases. The first phase, or sensitisation, occurs when nickel initially enters the body. There is usually no response present at this time but the immune system is primed or sensitised for an allergic response. The major sensitisation routes are nickel-containing jewellery and foods. Foods that are high in nickel include chocolate, soy beans, nuts and oatmeal. A response, or the elicitation phase, is in the form of a contact mucositis or dermatitis that occurs during re-exposure to nickel and develops over a period of days or rarely up to three weeks. If nickel is leached from orthodontic appliances, this Type IV hypersensitivity reaction cans occur.5, 6
Prevalence of Nickel Allergy
Nickel allergy occurs more frequently than allergy to all other metals combined.5 The incidence of Ni induced side effects from orthodontic materials in non-sensitized people is not known. It has also been suggested that the risk of sensitization from orthodontically derived Ni in these patients is extremely low. Nickel allergy is the most common contact allergy in industrialized countries; patch test verified data of general populations in several studies have shown that this allergy affects 10%30% of females and 13% of males.7, 8
This is thought to be due to ear piercing being a major cause of sensitization to nickel, as prevalence in subjects with pierced ears was 31% and those without pierced ears was 2%.9 People with cutaneous piercing were considered a significant risk factor for Ni allergy. Scientific evidence suggests that orthodontic treatment is not associated with increase of Ni
Hypersensitivity, unless patients have a history of previous cutaneous piercing exposure to Ni, usually ear piercing. Previous allergic history has been significantly associated by several authors to a hypersensitivity response to nickel released from orthodontic appliances.
Fortunately, most individuals who have nickel sensitivity do not report adverse clinical manifestations to orthodontic appliances containing nickel. It is estimated that the occurrence of a harmful response by patients to nickel is 0.1-0.2%.10 It is thought that a much greater concentration of nickel in the oral mucosa than the skin is necessary to elicit an allergic reaction.11 Nickel leaching of orthodontic bands, brackets and stainless steel or Ni-Ti arch-wires has been shown in vitro to maximally occur within the first week and then decline thereafter. This coincides with the approximate time frame for Type IV hypersensitivity reactions. Saliva or certain intraoral conditions such as foods, oral hygiene products and fluoride may potentially corrode the nickel in the alloy and release it onto the oral mucosa.
Clinical Features Associated With Allergy
Oral clinical signs and symptoms of nickel allergy can include the following: a burning sensation, gingival hyperplasia, labial desquamation, angular chelitis, erythema multiforme, periodontitis, stomatitis with mild to severe erythema, papularperi-oral rash, loss of taste or metallic taste, numbness, soreness at side of the tongue.12
These reactions are associated with an inflammatory response induced by corrosion of orthodontic appliances and subsequent release of nickel. It is manifested as Nickel Allergic Contact Stomatitis (NiACS). A burning sensation is the most frequent symptom. The aspect of the affected mucosa is also variable, from slight erythema to shiny lesions, with or without edema. In chronic cases, the affected mucosa is typically in contact with the causal agent and appears erythematous or hyperkeratoticto ulcerated.Extraoral manifestations of nickel allergy may have an intraoral origin.13
DIAGNOSIS
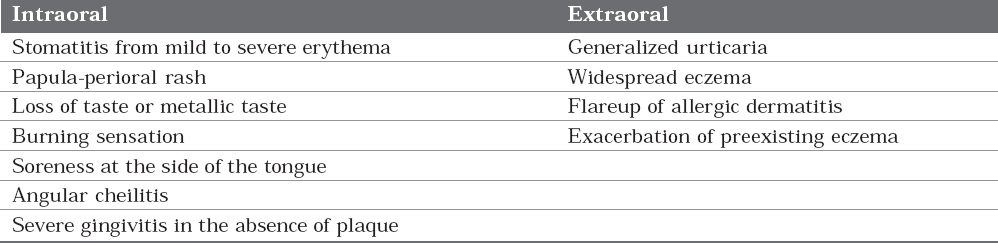
Sensitivity to nickel has been evaluated through biocompatibility tests, including cutaneous sensitivity (patch) tests,and reactivity to nickel has been evaluated with in vitro cell proliferation assays.The diagnosis of a response to nickel in the oral mucosa is more difficult than on the skin.It is important to make correct diagnosis of nickel allergy, symptoms of which may occur either within or remote to the oral environment. The signs and symptoms of nickel allergy are presented in Table 1.
|
Table 1: Signs and symptoms of nickel allergy14
Click here to view |
The following patient history would suggest a diagnosis of nickel allergy.14
-
Previous allergic response after wearing earrings or a metal watchstrap;
-
A known allergy to nickel should be determined when the patient completes the medical questionnaire or during a verbal medical history review
-
Appearance of allergy symptoms shortly after initial insertion of orthodontic components containing nickel;
-
Confined extra-oral rash adjacent to headgear studs.
A dermatologist should confirm the diagnosis by patch test in using 5% nickel sulfate in petroleum jelly.
A known allergy to nickel should be determined when the patient completes the medical questionnaire or during a verbal medical history review. The patient should then be forewarned of a possible response to the nickel in orthodontic appliances, particularly to the initial arch-wire placed.
MANAGEMENT OF NICKEL ALLERGY
Alternatives to Nickel-Titanium Wires
If intra-oral signs and symptoms are present and a diagnosis of nickel hypersensitivity is established, the nickel titanium arch-wire should be removed and replaced. Alternatives include:
-
Twist flex stainless steel
-
Fiber reinforced composite arch-wires
-
Wires such as TMA, pure titanium, and goldplated wires may also be used without risk.
-
Altered nickel-titanium arch-wires also exist and include plastic/resin coated nickel-titanium archwires.15
Ion-implanted nickel-titanium archwires have their surface bombarded with nitrogen ions, which forms an amorphous surface layer, conferring corrosion resistance and displacing nickel atoms, and decreasing the risk of an allergic response.
Stainless steel is slightly less expensive than Ni-Ti archwires while TMA is slightly more. Resin coated Ni-Ti wires are also an option. These resin- coated wires have had their surface treated with nitrogen ions, which forms an amorphous surface layer. Manufacturers claim that this results in an increase in corrosion resistance and decreased amount of leaching of nickel, more so than both NiTi and stainless steel wires.15
Most patients who develop a reaction to Ni-Ti archwires subsequently tolerate stainless steel without a reaction. This is believed to be a result of the nickel being tightly bound to the crystal lattice of the alloy, rendering them unable to be leached into the oral cavity. Stainless steel has been shown to release low amounts of nickel in artificial saliva or sweat which could help account for its low allergenicity.17
Incase, the patient continues to manifest an allergic reaction, the patient should be referred to a physician to be treated with antihistaminics, anaesthetics or topical corticosteroids.18
Attempts should be made to complete orthodontic treatment with TMA, fibre-reinforced composite, pure Ti or gold-plated wires.
Alternatives to Brackets
Stainless steel brackets are generally considered safe. However, nickel free alternative brackets to stainless steel include:
-
Ceramic brackets produced using polycrystalline alumina, single crystal sapphire, and zirconia;
-
Polycarbonate brackets that are produced from plastic polymers;
-
Titanium brackets;
-
Goldplated brackets;
-
Plastic aligners such as Invisalign™.
Extraoral metal components, including metal studs in headgear, are of greatest concern due to greater sensitivity of skin. Plastic coated headgear studs may be a better alternative for such patients.
The majority of investigations have found that nickel sensitive patients are able to tolerate stainless steel without any noticeable reaction.16 Most research concludes that stainless steel is a safe material to use for all intraoral orthodontic components for nickel sensitive patients.
CONCLUSION
Though an allergic response in the oral mucosa due to the nickel content from nickel containing orthodontic appliances is more infrequent than from nickel contact on the epidermis, it can still occur. If nickel-related intraoral clinical signs and symptoms appear, the orthodontist should be prepared to undertake or continue treatment without the use of Ni-Ti wires and even without stainless steel. . It is imperative for a practitioner to not only know the physical and mechanical properties of the materials being used, but also of the biologic compatibility of the material. Awareness of reactions that can occur with the various dental materials in treatment is important to the orthodontist. These materials can produce type IV hypersensitivity reactions. Diagnosis and treatment should include a multidisciplinary team. In all instances, the patient’s well-being should guide treatment decisions, and general health not just oral health should be the goal. Nevertheless when clinical signs and symptoms presumed to be due to nickel hypersensitivity are distressing to the patients, there are many alternatives available for the orthodontist. Safe and effective practice depends on identifying patients with allergy along with knowledge of materials that can potentially cause them.
